Abstract
Introduction: Urinary retention is a common emergency requiring immediate catheterization. Gradual decompression (GD) of the extended bladder is believed to minimize the risk of complications such as bleeding or circulatory collapse, but to date it has not been compared with rapid decompression (RD) in controlled trials. Materials and Methods: Male patients presenting with urinary retention (n = 294) were randomized to rapid or gradual catheterization. For the latter, the transurethral catheter was clamped for 5 min after every 200-ml outflow until the bladder was completely empty. Patients were monitored for at least 30 min thereafter with regular checks of vital signs and presence of macroscopic hematuria. Results: Of 294 patients, 142 (48.3%) were randomized to the GD and 152 (51.7%) to the RD group. Both groups showed no statistically significant difference with regard to age, anticoagulation treatment, catheter size and material, or volume retained. Hematuria occurred in 16 (11.3%) of the GD and 16 (10.5%) of the RD group; 6 patients in the former and 4 in the latter required further treatment. No circulatory collapse occurred. We noted a decrease in the previously raised blood pressure and heart rate in both groups, although without clinical significance. Conclusion: In this first randomized trial, no statistically significant difference was noted between gradual and rapid emptying of the bladder for urinary retention. Gradual emptying did not reduce the risk of hematuria or circulatory collapse. Therefore, there is no need to prefer gradual over rapid emptying, which is both easy and safe.
Introduction
Urinary retention is a common emergency which occurs in 2.2-6.8 men per 1,000 and increases with age [1,2,3]. In women, the incidence is not well documented [3]. Abdominal pain and the urge to void are symptomatic of acute retention. Chronic urinary retention develops over time with growing residual volumes and is often unnoticed by the patient [4]. Ultimately, however, this can lead to hydronephrosis and renal failure [5].
Initial management of urinary retention is drainage of the bladder by either transurethral or suprapubic catheterization. In most clinics, the transurethral approach is applied, primarily because it requires less training and is less invasive than suprapubic catheterization [6].
To date, debate persists over whether emptying should be rapid or gradual. Complications such as hematuria and circulatory collapse are thought to be increased by rapid decompression (RD) of an extended bladder [7,8], but gradual emptying is complex and time-consuming. In their 1997 review, Nyman et al. [9] found the complication rate in RD to be very low and therefore concluded that rapid emptying is safe. Nevertheless, urology textbooks and emergency guides for nurses and general practitioners continue to recommend gradual decompression (GD) to avoid complications [10,11].
To our knowledge, there are no controlled trials comparing the incidence of hematuria or circulatory collapse with both methods. Therefore, we conducted a prospective, randomized study to quantify and compare the risk of complications of RD and GD of the bladder in patients with urinary retention.
Materials and Methods
Patients and Randomization
After approval of our protocol by the Ethics Committee of the University of Witten/Herdecke, male patients presenting with symptoms of urinary retention (both acute and chronic) from April 2009 to August 2012 were enrolled after giving written informed consent to participate. Women and minors were excluded, as were patients with urethral strictures, suprapubic catheters and preexisting hematuria. Patients were randomized to RD or GD by drawing lots. Variables such as anticoagulation treatment, previous urogenital surgery, and catheter material and size were noted on the patient charts.
Treatment
Patients were assessed by a physician with brief history taking, clinical examination and ultrasound of the urinary tract. Ultrasound findings of hydronephrosis were classified as grade 1 with pelvic dilation only, grade 2 with accompanying mild calyceal dilation, grade 3 with severe calyceal dilation and grade 4 with calyceal dilation accompanied by renal parenchymal atrophy.
Catheter
We used an indwelling coudé-tipped catheter. The size and material were chosen with regard to patient history and known allergies. The catheter was placed by an experienced physician.
Bladder Emptying
For GD, after each 200 ml of urine drained, the catheter was clamped for 5 min and then reopened until the bladder was completely empty. For RD, the bladder was drained completely by placing the drainage bag at a lower level than the bladder. The volume was assessed using the scale on the bag.
Monitoring
After catheter placement, the patient was monitored for at least 30 min with regular checks of vital signs (heart rate and blood pressure). In case of hematuria, its severity and duration as well as necessary treatments were noted.
Further Treatment
Patients requiring additional treatment (e.g. for hematuria, infection, renal dysfunction and/or hydronephrosis) were admitted to hospital; all others were discharged with an indwelling catheter and referred to their general practitioner/urologist for a trial without catheter.
Statistics
Statistical evaluation of the data was done with SPSS. The Shapiro-Wilk test was used to test variables for normal distribution. For normally distributed variables, a two-tailed t test was used after confirmation of equal variances with the F test; for variables nonnormally distributed, the Mann-Whitney U test was applied. For all nonmetric variables, Fisher's exact test was used. All tests were performed for α = 0.05 on both sides.
Results
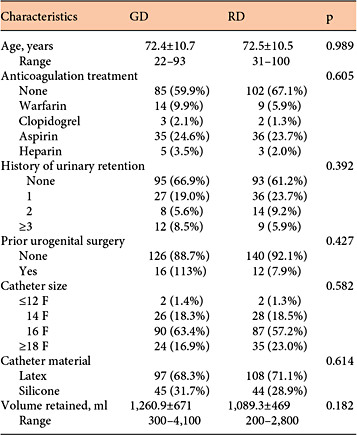
A total of 314 men were enrolled in our study, but due to missing data 20 were excluded from the analysis. Of 294 evaluable patients, 142 (48.3%) received GD and 152 (51.7%) RD. There were no statistically significant differences for possible confounding variables: age, anticoagulation treatment, history of urinary retention, previous urogenital surgery or catheter material and size (table 1). The retained volumes were slightly higher in the GD group (mean 1,260.9 ± 671 ml; range 300-4,100 ml) than in the RD group (mean 1,089 ± 469 ml; range 200-2,800 ml), but showed no statistically significant difference (p = 0.182).
Characteristics of the study patients (n = 294 men) undergoing catheterization for urinary retention
Before catheterization, hydronephrosis was found in 48.6% in the GD and 42.1% in the RD group. Grades I (19.7% GD vs. 17.1% RD) and II (18.3% GD vs. 15.3% RD) predominated, while severe hydronephrosis (grade III) was the least common (10.6% GD and 9.9% RD). There was no statistical difference in the frequency and grade of hydronephrosis between groups (p = 0.916). After complete emptying of the bladder, signs of hydronephrosis were found in 28.2% in the GD and 23.0% in the RD group.
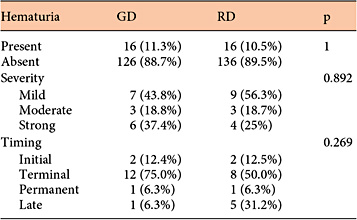
Bleeding complications after bladder decompression occurred in 16 (11.3%) patients in the GD and 16 (10.5%) in the RD group; 6 GD and 4 RD patients required intervention, but minor bleeding in the remainder ceased without further treatment. No statistical difference was found in the rate, severity or timing of bleeding (table 2).
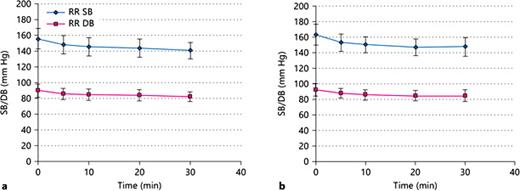
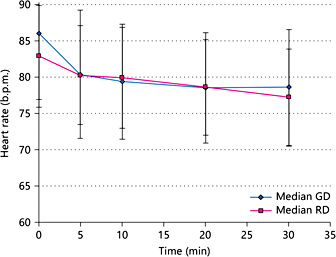
Before catheterization, blood pressure was elevated in both groups (GD mean 163/92 mm Hg; RD mean 157/90 mm Hg; pRRsys = 0.101, pRRdia = 0.334). During the monitoring period after catheterization, blood pressure decreased (GD 146/84 mm Hg and RD 142/82 mm Hg; pRRsys = 0.371, pRRdia = 0.264; fig. 1). Likewise, initial tachycardia (87/min GD and 84/min RD; p = 0.203)decreased during the follow-up in both groups (78/min GD and 78/min RD; p = 0.756; fig. 2). None of our 294 patients had circulatory collapse after catheterization.
Systolic (SB) and diastolic blood pressure (DB) levels (Riva-Rocci) of patients undergoing catheterization for urinary retention in the RD (a) and the GD group (b).
Systolic (SB) and diastolic blood pressure (DB) levels (Riva-Rocci) of patients undergoing catheterization for urinary retention in the RD (a) and the GD group (b).
Decrease in tachycardia during monitoring of patients undergoing catheterization.
Discussion
Our study found no advantage of GD over RD in urinary retention. To our knowledge, this is the first study to compare and quantify the complication rate of GD and RD of the bladder.
In their review of 1997, Nyman et al. [9] showed that postobstructive diuresis, blood pressure loss and hematuria are rare complications, allowing the conclusion that RD is safe. Nevertheless, recent reports continue to support the use of GD to avoid complications [11], and Fontanarosa and Roush [7] even recommend to slowly release chronic urinary retention over 24-36 h.
GD is more complex and time consuming for the attending nurses, physicians and patients than RD [5], and as yet no standard technique exists. Published methods vary: e.g. initial release of 500 ml followed by catheter clamping for 30 min with hourly release of 100-150 ml thereafter [5,12]; clamping after release of about 750 ml (favored by 57% of nurses in a 1990 survey) [9], or GD with an intravenous giving set [13].
Christensen et al. [14] evaluated intravesical pressure levels during GD and RD of an extended bladder in 10 patients and reported a decline to approximately 50% after release of the first 100 ml of urine. Although they concluded that GD should be done in steps smaller than 100 ml to allow a slower decline of intravesical pressure, this is inconvenient in clinical practice. In our study, we chose to release 200 ml every 5 min for GD, which is in line with the current practice and meets the requirements of clinical practice.
Our patient group represented the expected age range (median 72.5 ± 10 years) as the risk of urinary retention increases with advancing age: men aged 70-79 years have a 1:10 chance of urinary retention within the next 5 years, while in men >80 years the risk increases to 1:3 [2,4]. As urinary retention is very rare in women and has a complex etiology, women were not included in our trial.
We found no statistical difference between both study groups concerning possible confounding factors such as history of urinary retention, anticoagulation treatment, previous surgery, and catheter size and material as well as grade of hydronephrosis before or after catheterization.
The retained volume was estimated using the scale on the drainage bag. Although this measurement technique may not be exact, the available data allowed comparison as volumes were relatively high: a median of 1,260.9 ± 671 ml in the GD group and 1,089.3 ± 469 ml in the RD group. Other published studies stated similar volumes with a mean of 1,145 ml (500-2,200 ml) [15], 1,125 ml (450-3,100 ml) [14] and a range of 1,050-1,950 ml [16], and all reported a low incidence of RD complications.
Hematuria after decompression is believed to result from the sudden filling of compressed vessels with renal and bladder bleeding [5,8]. Animal studies have shown that urinary retention with raised intravesical pressure leads to tissue damage with edema and hemorrhage [17,18]. This leads to the conclusion that hematuria after treatment of urinary retention results from the degree of tissue damage rather than the mode of decompression, indicating that GD of an extended bladder prolongs patient suffering and possibly increases the risk of impairments in urinary and renal function [17]. Hematuria can also arise from other causes, e.g. catheterization trauma to the urethra, bladder cancer and infection.
Previous studies stated hematuria rates only for RD (2-16%) [9], with data lacking for GD. In our study, we found hematuria rates of 11.3 and 10.5% in both groups, with no significant difference in the degree, time of occurrence or duration. In both groups, a small number of patients required further interventional treatment (6 in the GD and 4 in the RD group). In all but 1 patient, hematuria was managed by irrigation and ceased within 2 days. One RD patient with a volume retention of 2,200 ml had severe renal failure owing to chronic retention with uremic platelet dysfunction [19] and extended bleeding and blood loss. After restoration of renal function and supportive treatment, this patient survived and was ultimately treated with subvesical de-obstruction surgery.
Another assumed complication of RD is circulatory collapse owing to viscerovascular reflexes: the overdistended bladder leads to hypertension from increased arterial wall tonus and vasoconstriction through the sympathetic nerve-mediated vesicovascular reflex. With bladder emptying, the reflex ceases along with a decline in blood pressure [14]. All available studies show normalization of a previously raised blood pressure after RD and ascribe this resolution to the fact that the patients originally presented in pain [9,14] or with hypertension owing to high-pressure chronic retention [20]. Our study supports these findings. Furthermore, we found no difference between RD and GD. Some patients showed pathologically high blood pressure levels before and after decompression. As data on preexisting hypertension were not recorded before decompression, we cannot assume that hypertension was solely the result of urinary retention.
Heart rate also decreased after decompression, with no statistical difference between groups. Of our 294 patients, none suffered from circulatory collapse in either group.
Conclusion
Our results show that GD for urinary retention does not minimize the risk of hematuria and circulatory collapse. In accord with previous reports, we recommend the use of RD as an easy and safe method for the relief of urinary retention.
References
This paper was presented at the 2012 Annual Conference of the Deutsche Gesellschaft für Urologie and was awarded the 1. Poster Prize.