Abstract
Introduction: The workload for benign prostatic hyperplasia (BPH) surgery is expected to rise with an increase in life expectancy and a growing population. Surgical modalities for BPH have evolved, shifting toward minimally invasive transurethral procedures. This study aimed to investigate the trends in BPH surgical procedures across medical centers in Israel. Methods: Data from seven academic medical centers in Israel from 2010 to 2022 were analyzed. Procedures included open prostatectomy, transurethral prostatectomy (TURP), holmium laser enucleation of the prostate (HoLEP), and photovaporization of the prostate (PVP). Statistical analyses were employed, including t tests, ANOVA, and ARIMA models. Results: Over 12 years, 13,478 BPH procedures were performed. TURP was the most common (72%), followed by open surgery (12%), HoLEP (12%), and PVP (3%). Annual procedures increased by approximately 5% each year, with a cumulative surge of 63% cases by 2022. The average patient’s age remained stable. TURP and HoLEP showed continual growth, while open surgery declined. HoLEP exhibited a shorter length of hospital stay compared to other modalities. Predictive models suggest open prostatectomy will cease within 2 years, while TURP and HoLEP will continue to rise. Conclusion: This study highlights a significant increase in BPH surgical procedures over time, with a notable preference for TURP and HoLEP. The findings emphasize the importance of size-independent techniques like HoLEP for optimal healthcare management in the future.
Introduction
Clinical benign prostatic hyperplasia (BPH) is estimated to affect nearly one in four men over their lifetime [1]. It is estimated that half of men aged 50 and older experience lower urinary tract symptoms attributed to BPH, with this figure escalating to 80% among men aged 70 and above [2, 3]. Symptomatic BPH can be managed conservatively through approaches such as watchful waiting, dietary adjustments, lifestyle modifications, and various medications. Surgical intervention becomes necessary when conservative and medical modalities fail to alleviate symptoms or when absolute indications arise. This includes urinary retention, the necessity for indwelling catheterization, recurrent infections, bladder stone formation, recurrent prostatic bleeding, and obstructive uropathy [4, 5].
Over the past 2 decades, surgical management options for BPH have undergone significant refinements, marked by introducing diverse energy sources and novel technologies. Moreover, there is a discernible trend toward transurethral interventions, irrespective of prostate size, while adhering to the principles of anatomical endoscopic enucleation of the prostate [6]. Our study explored the ongoing trends in BPH surgical procedures within academic medical institutions.
Patients and Methods
Study Design
The study received approval from the Internal Review Board at TLVMC (TLV No. 0317-22) for the principal investigator. Data were gathered from seven academic medical centers across Israel from 2010 to 2022. All seven medical centers are academic teaching hospitals, four are large referral centers, and two of the institutions are in rural areas. All men undergoing procedures for BPH were included in the analysis. Forty-two cases of patients enrolled in a clinical pilot study evaluating the safety and efficacy of the minimally invasive “Butterfly Medical Prostatic Retraction Device” (ClinicalTrials.gov Identifier: NCT03912558 [7, 8]) were excluded. Our medical system is served by four public and one military healthcare provider, comprehensively covering BPH surgeries at the medical centers included in this study. The rate of switching between healthcare providers in our region stands as low as 2%, while the country’s immigration rate is 2% [9, 10].
Data Acquisition
Data were retrieved from electronic files using MDClone, a data extraction and synthesis platform that provides patient data surrounding an index event (http://www.mdclone.com). Procedures were categorized into open prostatectomy (comprising retropubic and suprapubic prostatectomy), transurethral prostatectomy (TURP), holmium laser enucleation of the prostate (HoLEP), green laser photovaporization of the prostate (PVP), and other procedures. The data were then stratified into totals by year, type of surgery, age at the time of procedure, and length of hospital stay (LOS). We manually verified 10% of the cases to validate our data further, given that digital data extraction was employed.
Statistical Analysis
We used a t test and analysis of variance (ANOVA) to assess differences in continuous variables over the study duration between the groups. Additionally, a pooled analysis was performed on the number of procedures conducted annually by the procedure group. Changes in the annual total number of surgeries were calculated, along with the overall cumulative increase over the 12-year study period. ARIMA models were performed to predict trends in forthcoming years. All analyses were 2-sided, and statistical significance was p < 0.05. The analyses used Python 3.6.5, SPSS v. 29 (IBM, USA), and Excel 2017.
Results
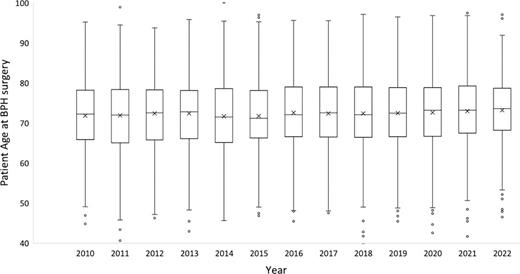
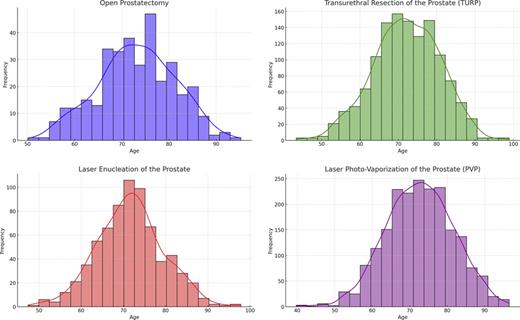
Table 1 presents the number of procedures, patient age, and LOS for individuals who underwent surgical interventions for BPH. Over 12 years, a total of 13,478 operations were conducted. TURP accounted for the majority of procedures with 9,916 cases (72%), followed by open surgery consisting of 1,644 cases (12%), HoLEP with 1,542 cases (12%), and 373 cases (3%) of PVP. A mere 4 cases (0.03%) fell into the “Other procedures” category, specifically transurethral incision of the prostate. Given the negligible number of cases, they were excluded from further analysis of procedure group types. Data on patient age were available for all patients. Age was distributed normally (Shapiro-Wilk test, p > 0.05); the mean and standard deviation (SD) were calculated. The average age at the time of the procedure of the entire cohort was 72.4 ± 8.9 years. Given the normal distribution of patient age, we used a one-way ANOVA to compare the average patient’s age between the years. Throughout the study period, the average age remained relatively stable, with no significant differences over the years (p < 0.05) (Fig. 1). Age distribution for each procedure separately was calculated and found to be distributed normally (Fig. 2). The average age among open surgery was the oldest (73 ± 8.0), followed by TURP (72.4 ± 9.0), PVP (72 ± 9.9), and lastly, HoLEP (70.4 ± 8.4). The average age at the time of the procedure was significantly lower in HoLEP compared to open prostatectomy and TURP (p < 0.05).
Number of procedures, patient age, and LOS categorized by procedure type
| Procedure . | Procedures, n (N = 13,478) . | Age, years (mean±SD) (N = 13,478) . | LOS, days (mean±SD) (N = 12,163) . |
|---|---|---|---|
| Overall | 13,478 | 72.2±8.9 | 3.5±5.8 |
| TURP | 9,916 (73%) | 72.4±9.0 | 3.1±4.9 |
| Open surgery | 1,644 (12%) | 73.0±8.0 | 6.5±5.5 |
| HoLEP | 1,542 (12%) | 70.4±8.4 | 1.6±1.4 |
| PVP | 373 (3%) | 72.0±9.9 | NA |
| Procedure . | Procedures, n (N = 13,478) . | Age, years (mean±SD) (N = 13,478) . | LOS, days (mean±SD) (N = 12,163) . |
|---|---|---|---|
| Overall | 13,478 | 72.2±8.9 | 3.5±5.8 |
| TURP | 9,916 (73%) | 72.4±9.0 | 3.1±4.9 |
| Open surgery | 1,644 (12%) | 73.0±8.0 | 6.5±5.5 |
| HoLEP | 1,542 (12%) | 70.4±8.4 | 1.6±1.4 |
| PVP | 373 (3%) | 72.0±9.9 | NA |
HoLEP, holmium laser enucleation of prostate; LOS, length of hospital stay; PVP, photovaporization of the prostate; SD, standard deviation; TURP, transurethral prostatectomy.
Average patient age for all BPH procedure types (N = 13,478) by year. BPH, benign prostatic hyperplasia.
Average patient age for all BPH procedure types (N = 13,478) by year. BPH, benign prostatic hyperplasia.
Data regarding LOS of the 373 PVP cases (10%) were missing and were available for the rest of the cases (N = 12,163, 90% of the cohort). LOS was distributed normally (Shapiro-Wilk test, p > 0.05); the mean and SD were calculated. The overall average LOS was 3.5 ± 5.8 days. The average LOS of HoLEP was 1.6 ± 1.4 days, significantly shorter (p < 0.05) compared to open surgery (6.5 ± 5.5) and TURP (3.1 ± 4.9).
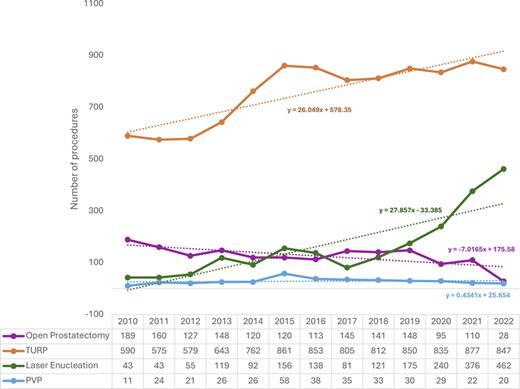
Temporal trends are presented and depicted in Figure 3. On average, the total number of procedures exhibited a 5% annual increase, leading to a cumulative rise from 833 procedures in 2010 to 1,357 procedures in 2022, marking a 63% increase over the 12 years. The number of TURPs increased steadily over the years, from 590 procedures in 2010 to 847 in 2022, maintaining its status as the most common BPH procedure throughout the study period. PVP procedures remained consistent over the study duration, ranging from 11 to 58 procedures per year. Open prostatectomies declined negatively (slope = −7), starting at 189 procedures in 2010 and decreasing to 28 in 2022. In contrast, laser enucleation demonstrated an upward trend during the study period, with a positive linear incline (slope = +28), beginning at 43 in 2010 and reaching 462 in 2022. Since 2019, the trend of laser prostatectomy surpassed that of the open procedure (175 vs. 148). For each procedure (open surgery, TURP, HoLEP, and PVP), the hospital analyzed data to detect anomalies that could serve as confounding factors using a two-way ANOVA. No significant differences were found between hospitals regarding patients’ age and LOS (p < 0.05).
Temporal trends of BPH procedures between 2010 and 2022, categorized by procedure type. PVP, photovaporization of the prostate; TURP, transurethral prostatectomy.
Temporal trends of BPH procedures between 2010 and 2022, categorized by procedure type. PVP, photovaporization of the prostate; TURP, transurethral prostatectomy.
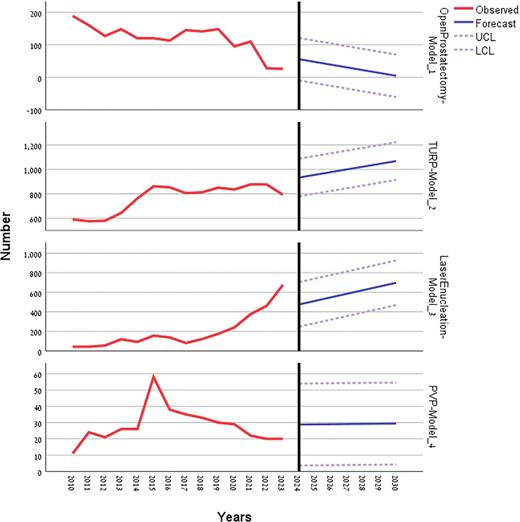
Utilizing ARIMA models, we have generated forecasts projecting the expected trends for each procedure type over the next decade (Fig. 4). Based on our predictive models, it is anticipated that open prostatectomy will cease to be performed within the next 2 years. Meanwhile, the frequency of PVP procedures is expected to remain stable at approximately 20 annual procedures. Furthermore, both TURP and HoLEP procedures are projected to experience continual growth, reaching an estimated 1,050 and 1,400 procedures by 2032. Notably, HoLEP is anticipated to exhibit a steeper incline, gradually closing the gap with TURP and becoming more abundant within 6 years (1,028 vs. 975 procedures).
Projected numbers of BPH procedures for the upcoming years in Israel. HoLEP, holmium laser enucleation of prostate; PVP, photovaporization of the prostate; TURP, transurethral prostatectomy.
Projected numbers of BPH procedures for the upcoming years in Israel. HoLEP, holmium laser enucleation of prostate; PVP, photovaporization of the prostate; TURP, transurethral prostatectomy.
Discussion
In this retrospective pooled analysis, we investigated the temporal trends in the surgical modalities for BPH across seven academic medical centers in Israel. Over 12 years, we noted a consistent average age among patients undergoing surgery despite observing an annual increase of 5% and a cumulative workload surge of 63% in BPH surgeries. Open surgery has been largely replaced by HoLEP, which has a significantly shorter LOS than other modalities and is predicted to dominate among BPH procedures in less than 10 years.
Our findings align with prior studies that have observed a growing burden of BPH/LUTS globally as the population ages [11, 12]. However, we did not observe a trend or alteration in patient age during surgery over the study period. The increased density of urologists may elucidate this observation as it may improve access to healthcare services and expand the population size without a corresponding shift in the age at which symptoms peak. Currently, a wide range of surgical options exists for managing BPH, encompassing procedures such as open prostatectomy, TURP, HoLEP, and PVP, among others. However, selecting the most suitable treatment can pose a challenge. Guidelines from the American Urological Association (AUA) and the European Association of Urology (EAU) provide recommendations based on prostate size, with TURP or PVP being recommended for patients with prostates ranging from 30 to 80 cc. For larger prostates exceeding 80 cc, modalities involving adenoma enucleation, such as open prostatectomy and HoLEP, are suggested.
Despite HoLEP being associated with a relatively steep learning curve [13, 14], our study suggests a growing preference for HoLEP over open prostatectomy and TURP. Several factors may account for this trend. While open prostatectomy is typically reserved for larger prostates, HoLEP is highlighted as a size-independent option and has demonstrated excellent and durable outcomes, even over a follow-up period of 20 years [15]. Furthermore, compared to open prostatectomy, HoLEP is associated with lower rates of overall and major postoperative complications, including reduced need for blood transfusions and less invasive interventions [16‒19]. Although HoLEP yields functional outcomes equivalent to TURP, it has shown superior cost-effectiveness across varying severities of BPH [20, 21], reflected in our study by the shorter LOS. These advantages of HoLEP make it a more appealing choice for urologists when considering treatment options for their BPH patients.
This study is subject to certain limitations inherent in its retrospective design. Selection bias may have been introduced as retrospective studies rely on pre-existing data rather than prospectively collected information. Furthermore, our analysis did not include other minimally invasive surgery techniques, such as Rezūm, Urolift, or robotic simple prostatectomy, as they are currently only accessible through private insurance rather than the public-funded healthcare system from which our data were derived. Data quality and consistency from different sources may also vary, potentially introducing confounding variables. Despite these limitations, the participation of seven geographically diverse teaching hospitals enhances the robustness of our findings, reflecting heterogeneity in both the population and clinical practices.
Conclusion
As the global population continues to age, the prevalence of BPH is anticipated to rise, highlighting the importance of taking a proactive approach to adopt newer surgical strategies and plan for potential strains on healthcare resources in the future. The escalating BPH workload underscores the need to transition toward endoscopic size-independent surgical techniques to optimize resource management.
Statement of Ethics
The study received approval from the Internal Review Board at Tel Aviv Medical Center (TLV No. 0317-22). As the present study was carried out retrospectively, the need to obtain written informed consent from the patients was waived by the Institutional Review Board. Personal identifiers of the patients were removed, and the data were analyzed anonymously.
Conflict of Interest Statement
The authors declare that they have no competing interests.
Funding Sources
The authors received no financial support for the research, authorship, and/or publication of this article. No competing financial interests exist.
Author Contributions
Conception and design – Karin Lifshitz and Mario Sofer. Acquisition of data – Hen Hendel, Yaron Ehrlich, Omer Anis, Zohar Dotan, Guy Verhovsky, Ehud Genessin, Rabeea Moed, Nicola Mabjeesh, Mahmoud Abbas, Ilan Kafka, Ali Safadi, and Ran Katz. Analysis and interpretation – Karin Lifshitz, Ziv Savin, Ofer Yossepowitch, and Mario Sofer. Drafting of the manuscript – Karin Lifshitz. Critical revision of the manuscript – Ziv Savin, Ofer Yossepowitch, and Mario Sofer. Statistical analysis – Karin Lifshitz, Tomer Bashi, Snir Dakelo, and Ziv Savin. Supervision – Mario Sofer.
Data Availability Statement
The complete data supporting this study’s findings are not publicly available due to the privacy of research participants but are available from the corresponding author, Dr. Karin Lifshitz.