Abstract
Introduction: Our study aimed to assess the independent and joint effects of leisure-time physical activity and sedentary behavior with urinary incontinence (UI). Methods: Data were obtained from the National Health and Nutrition Examination Survey 2011–2016. The primary endpoint was the risk of different subtypes of UI, including stress UI, urgency UI, and mixed UI. The primary exposures were leisure-time physical activity and sedentary behavior. Sedentary behavior was assessed by screen time. Weighted univariate and multivariate logistic regression models were used to observe the independent and joint relationship of leisure-time physical activity and sedentary behavior with UI risk (including stress UI, urgency UI, and mixed UI). Results: In total, 6,927 female participants were included in this analysis. 3,377 females did not have UI, 1,534 had stress UI, 836 had urgency UI, and 1,180 had mixed UI. Screen time with ≥5 h/day was associated with increased odds of urgency UI (odds ratio [OR] = 1.31, 95% confidence intervals (CI): 1.06–1.61), which indicated the relationship of sedentary behavior and urgency UI. Engaging in leisure-time physical activity with of ≥750 metabolic equivalent (MET)·min/week was found to be significantly associated with reduced likelihood of mixed UI (OR = 0.68, 95% CI: 0.55–0.85). Additionally, the interaction term of leisure-time physical activity<750 MET·min/week and screen time ≥5 h/day was observed to be linked with increased odds of urgency and mixed UI. Conclusion: Participants experiencing a lower level of leisure-time physical activity and a higher level of sedentary behavior together might enhance the urgency and mixed UI risk.
Introduction
Urinary incontinence (UI), which refers to the involuntary or unintentional leakage of urine, encompasses three main subtypes: stress, urgency, and mixed UI [1]. UI is a prevalent issue among women globally, resulting in detrimental physical and psychological consequences while imposing significant social and economic burdens [2]. A representative study conducted in the USA revealed that 61.8% of women experience UI [3]. Therefore, the identification of modifiable influencing factors holds significant clinical value in the prevention of female UI.
Pelvic floor muscle training and lifestyle modification have been recommended as the first-line treatment for all UI subtypes [4]. Physical activity serves as a crucial way for pelvic floor muscle training, and it also constitutes one of the common lifestyle modifications [5]. Existing evidence suggested that leisure-time physical activity, rather than occupational physical activity, is beneficial for human health [6, 7]. Data from Australian Longitudinal Study of Women’s Health indicated that higher level of leisure-time physical activity was correlated with a decreased risk of UI among young women, and engaging in appropriate physical activity may mitigate the risk of UI-related to obesity [8]. Besides physical activity, there is an increasing concern regarding the adverse health impacts of sedentary behavior [9, 10]. Screen time is considered a significant indicator of sedentary behavior, and individual with screen time greater than 5 h/day had a similar risk of cardiovascular disease (CVD) as those with sedentary time exceeding 10 h/day [11]. A health survey pointed out that TV and/or screen watching for a duration of ≥6 h has been linked to the development of bladder disease, while a duration of ≥8 h has been connected to the genitourinary system disorders [12]. A recent cohort study conducted in the USA revealed a synergistic impact of insufficient levels of leisure-time physical activity and prolonged sedentary behavior on mortality risk [13]. Nevertheless, few study have provided insight into the joint effect of leisure-time physical activity and sedentary behavior on the UI risk. Herein, our study aimed to assess the independent and joint associations of leisure-time physical activity and sedentary behavior with the female UI risk, which provide certain references for the prevention of female UI.
Methods
Study Population
We performed a cross-sectional study utilizing data from National Health and Nutrition Examination Survey (NHANES) 2011–2016. NHANES is a cross-sectional and nationally representative study by using multistage stratified probability sampling design, intending to evaluate the nutritional and health status of the overall US population [14]. NHANES gathered data of subjects through interviews, physical examinations, and laboratory tests. NHANES protocol was approved by the Institutional Review Board of National Centers for Health Statistics (NCHS), with informed consent obtained from all participants.
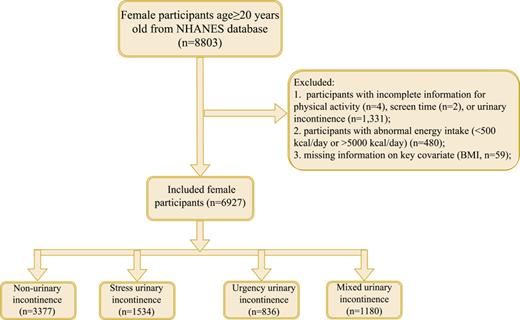
This study included female participants age ≥20 years old (n = 8,803). Then, some participants who had incomplete information for physical activity (n = 4), screen time (n = 2), or UI (n = 1,331) were excluded from the analysis. In addition, we also excluded participants with abnormal energy intake (<500 kcal/day or >5,000 kcal/day) (n = 480) or missing information on key covariates (n = 59). The analysis ultimately included 6,927 female participants as analytic samples. Figure 1 shows the flowchart of population selection.
Variables Collection
The primary endpoint was the occurrence of different subtypes of UI, including stress UI, urgency UI, and mixed UI. For NHANES participants, questionnaire data on “Kidney Condition” assessed the occurrence of UI [15]. Stress UI was defined as a positive response (yes) to the question, “During the past 12 months, have you leaked or lost control of even a small amount of urine with activity like coughing, lifting, or exercise?” Urgency UI was defined on the basis of the question (yes), “During the past 12 months, have you leaked or lost control of even a small amount of urine with an urge or pressure to urinate and you could not get to the toilet fast enough?” Mixed UI was defined as the presence of both stress and urgency UI.
Leisure-time physical activity was assessed through the Global Physical Activity Questionnaire. Leisure-time physical activity was converted to metabolic equivalent (MET) minutes of moderate to vigorous physical activity per week according to the World Health Organization analysis guide [16]. NHANES provides the recommended MET values for each physical activity. Leisure-time physical activity ≥750 MET·min/week is the ideal level [17]. Participants were assigned to two groups: <750 MET·min/week and ≥750 MET·min/week.
Sedentary behavior was assessed by screen time [11]. Screen time was based on self-reported total hours per day spent on watching TV and use of computer: (1) “Over the past 30 days, on average, how many hours per day did you sit and watch TV or video?” (2) “Over the past 30 days, on average, how many hours per day did you use a computer or play computer games outside of work or school?” Those with ≥5 h/day of screen time are regarded as prolonged screen time.
Potential covariates were collected: age (years), race, body mass index (BMI) (kg/m2), cotinine (ng/mL), alcohol (gm), drink status, smoking status, occupational physical activity, transportation physical activity, menopausal status, hypertension, diabetes, dyslipidemia, CVD, pelvic infection, use of female hormones, diuretic, muscle relaxant, vaginal deliveries, cesarean deliveries, prior hysterectomy, tried to lose weight, caffeine (mg), and moisture (gm). Hypertension, diabetes, dyslipidemia, and CVD were diagnosed by self-reported or taking medicines.
Statistical Analysis
All statistical analysis was performed in SAS 9.4 software. The mean matching prediction method was employed to impute the missing variables, and a sensitivity analysis was conducted on the datasets before and after interpolation (online suppl. Table 1; for all online suppl. material, see https://doi.org/10.1159/000538339). Continuous variables were described using the mean (standard error) (mean [SE]), and weighted t test was employed for group comparisons. Categorical variables were presented as the number of cases and component ratio [n (%)], with group comparisons conducted using the χ2 test.
All potential covariates were identified by using weighted univariate logistic analysis (p < 0.05) (online suppl. Table 2). We used weighted univariate and multivariate logistic regression models to observe the independent and joint relationship of leisure-time physical activity and sedentary behavior with the female stress UI risk, and the control group was the female with non-stress UI. The independent and joint relationship of leisure-time physical activity and sedentary behavior with the female urgency UI risk was assessed by weighted univariate and multivariate logistic regression models, and the control group was the female with non-urgency UI. Similarly, univariate and multivariate logistic regression models to observe the independent and joint relationship of leisure-time physical activity and sedentary behavior with the female mixed UI risk, and the control group was the female with non-mixed UI. In addition, we also performed a subgroup analysis based on BMI. Odds ratio (OR) was calculated with 95% confidence intervals (CI). The statistical significance was set at p < 0.05 for this analysis.
Results
Characteristics of Study Population
After screening, a total of 6,927 females were included for the further analysis. The characteristics of study population are presented in Table 1. Of the total population, the mean age was 48.47 years. 3,377 females did not have UI, 1,534 had stress UI, 836 had urgency UI, and 1,180 had mixed UI. As shown in Table 1, the characteristics of female with different subtypes of UI were also displayed. The mean age was 42.92 years in female non-UI, 49.62 years for stress UI, 57.16 years for urgency UI, and 56.53 years for mixed UI. There were 473 individuals with stress UI had screen time ≥5 h/day, 322 individuals with urgency UI had screen time ≥5 h/day, and 455 patients with mixed UI had screen time ≥5 h/day. In addition, online supplementary Table 3 also indicated the characteristic comparisons between groups (stress UI group vs. non-stress UI group; urgency UI group vs. non-urgency UI group; mixed UI group vs. non-mixed UI group).
Characteristics of the patients according to the with or without and different subtypes of UI
| Variables . | Total (n = 6,927) . | Non-UI (n = 3,377) . | Stress UI (n = 1,534) . | Urgency UI (n = 836) . | Mixed UI (n = 1,180) . |
|---|---|---|---|---|---|
| Age, years, mean (SE) | 48.47 (0.40) | 42.92 (0.48) | 49.62 (0.44) | 57.16 (0.85) | 56.53 (0.53) |
| Race, n (%) | |||||
| White | 2,721 (67.58) | 1,160 (63.11) | 710 (73.69) | 331 (67.08) | 520 (71.43) |
| Black | 1,563 (11.57) | 805 (13.01) | 228 (6.89) | 290 (18.10) | 240 (10.05) |
| Other | 2,643 (20.85) | 1,412 (23.88) | 596 (19.42) | 215 (14.82) | 420 (18.51) |
| BMI, n (%) | |||||
| <18.5 kg/m2 | 127 (1.80) | 87 (2.47) | 12 (0.92) | 15 (1.62) | 13 (1.31) |
| 18.5–25 kg/m2 | 1,912 (29.77) | 1,164 (36.57) | 357 (26.34) | 177 (23.84) | 214 (19.74) |
| 25–30 kg/m2 | 1,897 (28.14) | 923 (28.20) | 469 (31.01) | 225 (27.92) | 280 (23.87) |
| ≥30 kg/m2 | 2,991 (40.28) | 1,203 (32.75) | 696 (41.73) | 419 (46.62) | 673 (55.08) |
| Drink status, n (%) | |||||
| Never | 2,727 (30.10) | 1,344 (30.28) | 566 (26.66) | 341 (34.28) | 476 (31.90) |
| <1 times/week | 1,575 (30.09) | 803 (32.34) | 352 (31.11) | 196 (28.15) | 224 (23.58) |
| ≥1 times/week | 2,053 (32.12) | 1,013 (31.91) | 476 (34.23) | 221 (28.15) | 343 (32.23) |
| Unknown | 572 (7.69) | 217 (5.47) | 140 (8.00) | 78 (9.42) | 137 (12.30) |
| Smoking status, n (%) | |||||
| No | 4,545 (62.08) | 2365 (65.93) | 967 (59.71) | 517 (60.66) | 696 (55.72) |
| Current smoking | 1,116 (16.66) | 506 (15.44) | 255 (17.47) | 122 (14.62) | 233 (20.26) |
| Quit smoking | 1,266 (21.26) | 506 (18.63) | 312 (22.81) | 197 (24.72) | 251 (24.03) |
| Occupational physical activity, MET·min/week, mean (SE) | 1,565.46 (67.11) | 1,678.22 (109.82) | 1,598.84 (105.26) | 1,310.22 (208.40) | 1,370.74 (105.35) |
| Transportation physical activity, MET·min/week, mean (SE) | 235.38 (15.60) | 282.55 (20.80) | 198.55 (18.97) | 176.89 (27.08) | 196.66 (36.69) |
| Menopausal status, n (%) | |||||
| No | 3,232 (47.64) | 1,936 (59.08) | 729 (47.16) | 246 (30.15) | 321 (27.94) |
| Yes | 2,532 (35.31) | 989 (27.11) | 549 (35.90) | 422 (50.59) | 572 (47.21) |
| Unknown | 1,163 (17.05) | 452 (13.81) | 256 (16.94) | 168 (19.26) | 287 (24.85) |
| Hypertension, yes, n (%) | 3,797 (51.53) | 1,521 (41.34) | 857 (53.13) | 582 (65.12) | 837 (68.68) |
| Diabetes, yes, n (%) | 1,187 (12.88) | 407 (8.35) | 270 (13.26) | 177 (14.76) | 333 (23.81) |
| Dyslipidemia, yes, n (%) | 4,536 (65.68) | 1,948 (57.03) | 1,064 (69.21) | 602 (72.66) | 922 (80.05) |
| CVD, yes, n (%) | 469 (5.85) | 134 (3.24) | 86 (4.99) | 88 (9.02) | 161 (12.32) |
| Pelvic infection, n (%) | |||||
| No | 3,039 (45.57) | 1,717 (52.69) | 699 (46.82) | 235 (29.62) | 388 (34.41) |
| Yes | 163 (2.32) | 55 (1.58) | 48 (2.90) | 24 (2.34) | 36 (3.56) |
| Unknown | 3,725 (52.11) | 1,605 (45.73) | 787 (50.28) | 577 (68.05) | 756 (62.03) |
| Use of female hormones, yes, n (%) | 1,555 (28.92) | 648 (25.31) | 354 (29.38) | 224 (35.50) | 329 (33.93) |
| Diuretic, yes, n (%) | 1,133 (14.66) | 423 (11.14) | 233 (13.89) | 202 (20.06) | 275 (22.09) |
| Muscle relaxant, yes, n (%) | 248 (4.13) | 78 (2.83) | 64 (4.40) | 34 (4.26) | 72 (7.31) |
| Vaginal deliveries, n (%) | |||||
| 0 | 1,124 (16.20) | 638 (18.89) | 234 (15.25) | 117 (14.32) | 135 (11.31) |
| 1 | 1,014 (15.37) | 485 (14.81) | 259 (17.65) | 116 (15.40) | 154 (13.55) |
| 2 | 1,460 (23.64) | 590 (18.88) | 403 (29.59) | 173 (21.66) | 294 (29.58) |
| 3 | 991 (13.41) | 401 (10.33) | 252 (15.88) | 131 (14.76) | 207 (17.53) |
| ≥4 | 1,129 (11.91) | 425 (8.54) | 241 (11.63) | 191 (19.35) | 272 (16.80) |
| Unknown | 1,209 (19.46) | 838 (28.56) | 145 (10.00) | 108 (14.51) | 118 (11.22) |
| Cesarean deliveries, n (%) | |||||
| No | 1,852 (25.85) | 765 (21.75) | 457 (28.79) | 259 (29.08) | 371 (30.86) |
| Yes | 1,400 (18.20) | 712 (19.26) | 327 (19.57) | 146 (13.94) | 215 (16.06) |
| Unknown | 3,675 (55.95) | 1,900 (58.99) | 750 (51.64) | 431 (56.97) | 594 (53.09) |
| Prior hysterectomy, yes, n (%) | 1,523 (22.05) | 533 (15.96) | 319 (20.65) | 269 (31.04) | 402 (35.18) |
| Tried to lose weight, n (%) | |||||
| No | 3,254 (44.18) | 1,655 (45.59) | 669 (42.11) | 380 (42.49) | 550 (44.42) |
| Yes | 2,726 (41.30) | 1,313 (41.42) | 632 (41.92) | 318 (41.69) | 463 (39.79) |
| Unknown | 947 (14.52) | 409 (12.99) | 233 (15.98) | 138 (15.82) | 167 (15.79) |
| Caffeine, n (%) | 154.82 (3.39) | 140.20 (4.58) | 165.66 (6.80) | 160.74 (10.31) | 175.95 (9.57) |
| <150 mg | 4,818 (61.86) | 2443 (65.16) | 1,004 (58.35) | 595 (60.52) | 776 (58.69) |
| 150–449 mg | 1,843 (32.51) | 831 (30.86) | 465 (36.03) | 204 (31.36) | 343 (32.73) |
| ≥450 mg | 266 (5.63) | 103 (3.98) | 65 (5.62) | 37 (8.12) | 61 (8.58) |
| Moisture, gm, mean (SE) | 2,828.75 (26.57) | 2,795.77 (37.65) | 2,836.52 (41.89) | 2,765.63 (67.82) | 2,952.75 (48.86) |
| Screen time, n (%) | |||||
| <5 h | 4,688 (68.06) | 2,378 (70.63) | 1,061 (70.73) | 514 (62.01) | 735 (60.93) |
| ≥5 h | 2,239 (31.94) | 999 (29.37) | 473 (29.27) | 322 (37.99) | 445 (39.07) |
| Leisure-time physical activity, n (%) | |||||
| <750 MET·min/week | 5,132 (70.05) | 2,367 (65.46) | 1,103 (68.26) | 666 (75.00) | 996 (82.30) |
| ≥750 MET·min/week | 1,795 (29.95) | 1,010 (34.54) | 431 (31.74) | 170 (25.00) | 184 (17.70) |
| Variables . | Total (n = 6,927) . | Non-UI (n = 3,377) . | Stress UI (n = 1,534) . | Urgency UI (n = 836) . | Mixed UI (n = 1,180) . |
|---|---|---|---|---|---|
| Age, years, mean (SE) | 48.47 (0.40) | 42.92 (0.48) | 49.62 (0.44) | 57.16 (0.85) | 56.53 (0.53) |
| Race, n (%) | |||||
| White | 2,721 (67.58) | 1,160 (63.11) | 710 (73.69) | 331 (67.08) | 520 (71.43) |
| Black | 1,563 (11.57) | 805 (13.01) | 228 (6.89) | 290 (18.10) | 240 (10.05) |
| Other | 2,643 (20.85) | 1,412 (23.88) | 596 (19.42) | 215 (14.82) | 420 (18.51) |
| BMI, n (%) | |||||
| <18.5 kg/m2 | 127 (1.80) | 87 (2.47) | 12 (0.92) | 15 (1.62) | 13 (1.31) |
| 18.5–25 kg/m2 | 1,912 (29.77) | 1,164 (36.57) | 357 (26.34) | 177 (23.84) | 214 (19.74) |
| 25–30 kg/m2 | 1,897 (28.14) | 923 (28.20) | 469 (31.01) | 225 (27.92) | 280 (23.87) |
| ≥30 kg/m2 | 2,991 (40.28) | 1,203 (32.75) | 696 (41.73) | 419 (46.62) | 673 (55.08) |
| Drink status, n (%) | |||||
| Never | 2,727 (30.10) | 1,344 (30.28) | 566 (26.66) | 341 (34.28) | 476 (31.90) |
| <1 times/week | 1,575 (30.09) | 803 (32.34) | 352 (31.11) | 196 (28.15) | 224 (23.58) |
| ≥1 times/week | 2,053 (32.12) | 1,013 (31.91) | 476 (34.23) | 221 (28.15) | 343 (32.23) |
| Unknown | 572 (7.69) | 217 (5.47) | 140 (8.00) | 78 (9.42) | 137 (12.30) |
| Smoking status, n (%) | |||||
| No | 4,545 (62.08) | 2365 (65.93) | 967 (59.71) | 517 (60.66) | 696 (55.72) |
| Current smoking | 1,116 (16.66) | 506 (15.44) | 255 (17.47) | 122 (14.62) | 233 (20.26) |
| Quit smoking | 1,266 (21.26) | 506 (18.63) | 312 (22.81) | 197 (24.72) | 251 (24.03) |
| Occupational physical activity, MET·min/week, mean (SE) | 1,565.46 (67.11) | 1,678.22 (109.82) | 1,598.84 (105.26) | 1,310.22 (208.40) | 1,370.74 (105.35) |
| Transportation physical activity, MET·min/week, mean (SE) | 235.38 (15.60) | 282.55 (20.80) | 198.55 (18.97) | 176.89 (27.08) | 196.66 (36.69) |
| Menopausal status, n (%) | |||||
| No | 3,232 (47.64) | 1,936 (59.08) | 729 (47.16) | 246 (30.15) | 321 (27.94) |
| Yes | 2,532 (35.31) | 989 (27.11) | 549 (35.90) | 422 (50.59) | 572 (47.21) |
| Unknown | 1,163 (17.05) | 452 (13.81) | 256 (16.94) | 168 (19.26) | 287 (24.85) |
| Hypertension, yes, n (%) | 3,797 (51.53) | 1,521 (41.34) | 857 (53.13) | 582 (65.12) | 837 (68.68) |
| Diabetes, yes, n (%) | 1,187 (12.88) | 407 (8.35) | 270 (13.26) | 177 (14.76) | 333 (23.81) |
| Dyslipidemia, yes, n (%) | 4,536 (65.68) | 1,948 (57.03) | 1,064 (69.21) | 602 (72.66) | 922 (80.05) |
| CVD, yes, n (%) | 469 (5.85) | 134 (3.24) | 86 (4.99) | 88 (9.02) | 161 (12.32) |
| Pelvic infection, n (%) | |||||
| No | 3,039 (45.57) | 1,717 (52.69) | 699 (46.82) | 235 (29.62) | 388 (34.41) |
| Yes | 163 (2.32) | 55 (1.58) | 48 (2.90) | 24 (2.34) | 36 (3.56) |
| Unknown | 3,725 (52.11) | 1,605 (45.73) | 787 (50.28) | 577 (68.05) | 756 (62.03) |
| Use of female hormones, yes, n (%) | 1,555 (28.92) | 648 (25.31) | 354 (29.38) | 224 (35.50) | 329 (33.93) |
| Diuretic, yes, n (%) | 1,133 (14.66) | 423 (11.14) | 233 (13.89) | 202 (20.06) | 275 (22.09) |
| Muscle relaxant, yes, n (%) | 248 (4.13) | 78 (2.83) | 64 (4.40) | 34 (4.26) | 72 (7.31) |
| Vaginal deliveries, n (%) | |||||
| 0 | 1,124 (16.20) | 638 (18.89) | 234 (15.25) | 117 (14.32) | 135 (11.31) |
| 1 | 1,014 (15.37) | 485 (14.81) | 259 (17.65) | 116 (15.40) | 154 (13.55) |
| 2 | 1,460 (23.64) | 590 (18.88) | 403 (29.59) | 173 (21.66) | 294 (29.58) |
| 3 | 991 (13.41) | 401 (10.33) | 252 (15.88) | 131 (14.76) | 207 (17.53) |
| ≥4 | 1,129 (11.91) | 425 (8.54) | 241 (11.63) | 191 (19.35) | 272 (16.80) |
| Unknown | 1,209 (19.46) | 838 (28.56) | 145 (10.00) | 108 (14.51) | 118 (11.22) |
| Cesarean deliveries, n (%) | |||||
| No | 1,852 (25.85) | 765 (21.75) | 457 (28.79) | 259 (29.08) | 371 (30.86) |
| Yes | 1,400 (18.20) | 712 (19.26) | 327 (19.57) | 146 (13.94) | 215 (16.06) |
| Unknown | 3,675 (55.95) | 1,900 (58.99) | 750 (51.64) | 431 (56.97) | 594 (53.09) |
| Prior hysterectomy, yes, n (%) | 1,523 (22.05) | 533 (15.96) | 319 (20.65) | 269 (31.04) | 402 (35.18) |
| Tried to lose weight, n (%) | |||||
| No | 3,254 (44.18) | 1,655 (45.59) | 669 (42.11) | 380 (42.49) | 550 (44.42) |
| Yes | 2,726 (41.30) | 1,313 (41.42) | 632 (41.92) | 318 (41.69) | 463 (39.79) |
| Unknown | 947 (14.52) | 409 (12.99) | 233 (15.98) | 138 (15.82) | 167 (15.79) |
| Caffeine, n (%) | 154.82 (3.39) | 140.20 (4.58) | 165.66 (6.80) | 160.74 (10.31) | 175.95 (9.57) |
| <150 mg | 4,818 (61.86) | 2443 (65.16) | 1,004 (58.35) | 595 (60.52) | 776 (58.69) |
| 150–449 mg | 1,843 (32.51) | 831 (30.86) | 465 (36.03) | 204 (31.36) | 343 (32.73) |
| ≥450 mg | 266 (5.63) | 103 (3.98) | 65 (5.62) | 37 (8.12) | 61 (8.58) |
| Moisture, gm, mean (SE) | 2,828.75 (26.57) | 2,795.77 (37.65) | 2,836.52 (41.89) | 2,765.63 (67.82) | 2,952.75 (48.86) |
| Screen time, n (%) | |||||
| <5 h | 4,688 (68.06) | 2,378 (70.63) | 1,061 (70.73) | 514 (62.01) | 735 (60.93) |
| ≥5 h | 2,239 (31.94) | 999 (29.37) | 473 (29.27) | 322 (37.99) | 445 (39.07) |
| Leisure-time physical activity, n (%) | |||||
| <750 MET·min/week | 5,132 (70.05) | 2,367 (65.46) | 1,103 (68.26) | 666 (75.00) | 996 (82.30) |
| ≥750 MET·min/week | 1,795 (29.95) | 1,010 (34.54) | 431 (31.74) | 170 (25.00) | 184 (17.70) |
UI, urinary incontinence; BMI, body mass index; PIR, poverty-income ratio; MET, metabolic equivalent; CVD, cardiovascular disease; Non-UI, without stress UI, urgency UI, or mixed UI.
Independent/Joint Effect of Leisure-Time Physical Activity and Sedentary Behavior with Stress UI
As shown in online supplementary Table 2, age, race, BMI, drink status, smoking status, transportation physical activity, menopausal status, hypertension, diabetes, dyslipidemia, CVD, pelvic infection, use of female hormones, muscle relaxant, vaginal deliveries, cesarean deliveries, prior hysterectomy, caffeine and tried to lose weight were regarded as the covariates related to stress UI (p < 0.05). In univariate model (model 1), there was no statistically significant difference observed between leisure-time physical activity and stress UI (p > 0.05). Screen time did not exhibit any association with stress UI (p > 0.05). Additionally, the combined analysis revealed no significant disparity between the mixed effects of leisure-time physical activity and sedentary behavior on stress UI (p > 0.05). These findings remained consistent even after adjusting for all potential confounding factors (Model 2, p > 0.05) (Table 2).
Independent/joint effect of leisure-time physical activity and sedentary behavior with stress UI
| Variables . | Model 1 . | Model 2A . | ||
|---|---|---|---|---|
| OR (95% CI) . | p value . | OR (95% CI) . | p value . | |
| Leisure-time physical activity | ||||
| <750 MET·min/week | Ref | Ref | ||
| ≥750 MET·min/week | 0.88 (0.73–1.06) | 0.172 | 1.11 (0.92–1.34) | 0.273 |
| Screen time | ||||
| <5 h | Ref | Ref | ||
| ≥5 h | 0.99 (0.82–1.20) | 0.956 | 0.93 (0.75–1.15) | 0.490 |
| Leisure-time physical activity and screen time | ||||
| ≥750 MET·min/week and <5 h | Ref | Ref | ||
| ≥750 MET·min/week and ≥5 h | 0.73 (0.53–1.01) | 0.055 | 0.78 (0.56–1.08) | 0.127 |
| <750 MET·min/week and <5 h | 1.03 (0.86–1.24) | 0.714 | 0.86 (0.71–1.03) | 0.106 |
| <750 MET·min/week and ≥5 h | 1.12 (0.86–1.47) | 0.390 | 0.85 (0.64–1.14) | 0.277 |
| Variables . | Model 1 . | Model 2A . | ||
|---|---|---|---|---|
| OR (95% CI) . | p value . | OR (95% CI) . | p value . | |
| Leisure-time physical activity | ||||
| <750 MET·min/week | Ref | Ref | ||
| ≥750 MET·min/week | 0.88 (0.73–1.06) | 0.172 | 1.11 (0.92–1.34) | 0.273 |
| Screen time | ||||
| <5 h | Ref | Ref | ||
| ≥5 h | 0.99 (0.82–1.20) | 0.956 | 0.93 (0.75–1.15) | 0.490 |
| Leisure-time physical activity and screen time | ||||
| ≥750 MET·min/week and <5 h | Ref | Ref | ||
| ≥750 MET·min/week and ≥5 h | 0.73 (0.53–1.01) | 0.055 | 0.78 (0.56–1.08) | 0.127 |
| <750 MET·min/week and <5 h | 1.03 (0.86–1.24) | 0.714 | 0.86 (0.71–1.03) | 0.106 |
| <750 MET·min/week and ≥5 h | 1.12 (0.86–1.47) | 0.390 | 0.85 (0.64–1.14) | 0.277 |
Model 1: univariate logistic regression model (no adjusted covariates).
Model 2A: multivariate logistic regression model, adjusting for age, race, body mass index, drink status, smoking status, transportation physical activity, menopausal status, hypertension, diabetes, dyslipidemia, cardiovascular disease, pelvic infection, use of female hormones, muscle relaxant, vaginal deliveries, cesarean deliveries, prior hysterectomy, caffeine and tried to lose weight.
UI, urinary incontinence; MET, metabolic equivalent; OR, odds ratio; CI, confidence interval.
Independent/Joint Effect of Leisure-Time Physical Activity and Sedentary Behavior with Urgency UI
Online supplementary Table 2 also shows the covariates related to urgency UI (p < 0.05), including age, smoking status, transportation physical activity, menopausal status, hypertension, diabetes, dyslipidemia, CVD, pelvic infection, use of female hormones, diuretic, vaginal deliveries, cesarean deliveries, prior hysterectomy and tried to lose weight. In the univariate analyses (Table 3), leisure-time physical activity with ≥750 MET·min/week was associated with decreased odds of urgency UI (OR = 0.63, 95% CI: 0.49–0.81, p < 0.001). Screen time with ≥5 h/day was associated with increased odds of urgency UI (OR = 1.47, 95% CI: 1.17–1.86, p = 0.001), which indicated that the relationship of sedentary behavior and urgency UI. After adjusting all covariates, we found the association of sedentary behavior and urgency UI remained (OR = 1.31, 95% CI: 1.06–1.61, p = 0.014). But there was no significant association for leisure-time physical activity and female urgency UI (p > 0.05). And importantly, the interaction term of leisure-time physical activity<750 MET·min/week and screen time ≥5 h/day was observed to be linked with increased odds of urgency UI after adjusting all covariates (OR = 1.53, 95% CI: 1.06–2.20, p = 0.023). The result indicated a joint effect of leisure-time physical activity and sedentary behavior on female urgency UI.
Independent/joint effect of leisure-time physical activity and sedentary behavior with urgency UI
| Variables . | Model 1 . | Model 2B . | ||
|---|---|---|---|---|
| OR (95% CI) . | p value . | OR (95% CI) . | p value . | |
| Leisure-time physical activity | ||||
| <750 MET·min/week | Ref | Ref | ||
| ≥750 MET·min/week | 0.63 (0.49–0.81) | <0.001 | 0.82 (0.63–1.06) | 0.133 |
| Screen time | ||||
| <5 h | Ref | Ref | ||
| ≥5 h | 1.47 (1.17–1.86) | 0.001 | 1.31 (1.06–1.61) | 0.014 |
| Leisure-time physical activity and screen time | ||||
| ≥750 MET·min/week and <5 h | Ref | Ref | ||
| ≥750 MET·min/week and ≥5 h | 1.31 (0.89–1.93) | 0.167 | 1.29 (0.86–1.94) | 0.215 |
| <750 MET·min/week and <5 h | 1.48 (1.12–1.96) | 0.007 | 1.19 (0.88–1.61) | 0.257 |
| <750 MET·min/week and ≥5 h | 2.14 (1.50–3.06) | <0.001 | 1.53 (1.06–2.20) | 0.023 |
| Variables . | Model 1 . | Model 2B . | ||
|---|---|---|---|---|
| OR (95% CI) . | p value . | OR (95% CI) . | p value . | |
| Leisure-time physical activity | ||||
| <750 MET·min/week | Ref | Ref | ||
| ≥750 MET·min/week | 0.63 (0.49–0.81) | <0.001 | 0.82 (0.63–1.06) | 0.133 |
| Screen time | ||||
| <5 h | Ref | Ref | ||
| ≥5 h | 1.47 (1.17–1.86) | 0.001 | 1.31 (1.06–1.61) | 0.014 |
| Leisure-time physical activity and screen time | ||||
| ≥750 MET·min/week and <5 h | Ref | Ref | ||
| ≥750 MET·min/week and ≥5 h | 1.31 (0.89–1.93) | 0.167 | 1.29 (0.86–1.94) | 0.215 |
| <750 MET·min/week and <5 h | 1.48 (1.12–1.96) | 0.007 | 1.19 (0.88–1.61) | 0.257 |
| <750 MET·min/week and ≥5 h | 2.14 (1.50–3.06) | <0.001 | 1.53 (1.06–2.20) | 0.023 |
Model 1: univariate logistic regression model (no adjusted covariates).
Model 2B: multivariate logistic regression model, adjusting for age, smoking status, transportation physical activity, menopausal status, hypertension, diabetes, dyslipidemia, cardiovascular disease, pelvic infection, use of female hormones, diuretic, vaginal deliveries, cesarean deliveries, prior hysterectomy, and tried to lose weight.
UI, urinary incontinence; MET, metabolic equivalent; OR, odds ratio; CI, confidence interval.
Independent/Joint Effect of Leisure-Time Physical Activity and Sedentary Behavior with Mixed UI
Similarly, the independent/joint effect of leisure-time physical activity and sedentary behavior with mixed UI was assessed in Table 4. After controlling for all covariates related to mixed UI (p < 0.05), engaging in leisure-time physical activity with ≥750 MET·min/week was found to be significantly associated with a reduced likelihood of female mixed UI (model 2: OR = 0.68, 95% CI: 0.55–0.85, p < 0.001). When examining the joint analysis, the interaction term of leisure-time physical activity <750 MET·min/week and screen time ≥5 h/day exhibited an association with an elevated likelihood of mixed UI in fully adjusted model (OR = 1.60, 95% CI: 1.15–2.21, p = 0.006). The findings suggest that there was a combined impact of engaging in leisure-time physical activity and sedentary behavior on female mixed UI.
Independent/joint effect of leisure-time physical activity and sedentary behavior with mixed UI
| Variables . | Model 1 . | Model 2C . | ||
|---|---|---|---|---|
| OR (95% CI) . | p value . | OR (95% CI) . | p value . | |
| Leisure-time physical activity | ||||
| <750 MET·min/week | Ref | Ref | ||
| ≥750 MET·min/week | 0.41 (0.33–0.50) | <0.001 | 0.68 (0.55–0.85) | <0.001 |
| Screen time | ||||
| <5 h | Ref | Ref | ||
| ≥5 h | 1.54 (1.23–1.93) | <0.001 | 1.14 (0.91–1.44) | 0.240 |
| Leisure-time physical activity and screen time | ||||
| ≥750 MET·min/week and <5 h | Ref | Ref | ||
| ≥750 MET·min/week and ≥5 h | 1.07 (0.68–1.70) | 0.758 | 1.00 (0.60–1.65) | 0.993 |
| <750 MET·min/week and <5 h | 2.14 (1.69–2.72) | <0.001 | 1.39 (1.03–1.89) | 0.031 |
| <750 MET·min/week and ≥5 h | 3.22 (2.37–4.39) | <0.001 | 1.60 (1.15–2.21) | 0.006 |
| Variables . | Model 1 . | Model 2C . | ||
|---|---|---|---|---|
| OR (95% CI) . | p value . | OR (95% CI) . | p value . | |
| Leisure-time physical activity | ||||
| <750 MET·min/week | Ref | Ref | ||
| ≥750 MET·min/week | 0.41 (0.33–0.50) | <0.001 | 0.68 (0.55–0.85) | <0.001 |
| Screen time | ||||
| <5 h | Ref | Ref | ||
| ≥5 h | 1.54 (1.23–1.93) | <0.001 | 1.14 (0.91–1.44) | 0.240 |
| Leisure-time physical activity and screen time | ||||
| ≥750 MET·min/week and <5 h | Ref | Ref | ||
| ≥750 MET·min/week and ≥5 h | 1.07 (0.68–1.70) | 0.758 | 1.00 (0.60–1.65) | 0.993 |
| <750 MET·min/week and <5 h | 2.14 (1.69–2.72) | <0.001 | 1.39 (1.03–1.89) | 0.031 |
| <750 MET·min/week and ≥5 h | 3.22 (2.37–4.39) | <0.001 | 1.60 (1.15–2.21) | 0.006 |
Model 1: univariate logistic regression model (no adjusted covariates).
Model 2C: multivariate logistic regression model, adjusting for age, race, body mass index, drink status, smoking status, menopausal status, hypertension, diabetes, dyslipidemia, cardiovascular disease, pelvic infection, use of female hormones, diuretic, muscle relaxant, vaginal deliveries, cesarean deliveries, prior hysterectomy, caffeine, tried to lose weight and moisture.
UI, urinary incontinence; MET, metabolic equivalent; OR, odds ratio; CI, confidence interval.
Subgroup Analysis
Table 5 shows the result of subgroup analysis based on BMI. For females with BMI <25 kg/m2, leisure-time physical activity with ≥750 MET·min/week was only associated with decreased odds of mixed UI (OR = 0.58, 95% CI: 0.35–0.96, p = 0.036). Joint analysis indicated that the interaction term of leisure-time physical activity <750 MET·min/week and screen time ≥5 h/day exhibited an association with an elevated likelihood of urgency UI (OR = 1.67, 95% CI: 1.05–2.68, p = 0.032) and mixed UI (OR = 1.75, 95% CI: 1.01–3.04, p = 0.045). While for females with BMI ≥25 kg/m2, leisure-time physical activity showed only an association with mixed UI, and the combined effect of leisure-time physical activity and sedentary behavior was also observed exclusively for mixed UI.
Subgroup analysis
| Outcomes . | Variables . | BMI: <25 kg/m2 . | BMI: ≥25 kg/m2 . | ||
|---|---|---|---|---|---|
| OR (95% CI) . | p value . | OR (95% CI) . | p value . | ||
| (1) Stress UI | Leisure-time physical activity | ||||
| <750 MET·min/week | Ref | Ref | |||
| ≥750 MET·min/week | 1.06 (0.69–1.62) | 0.801 | 1.09 (0.88–1.36) | 0.407 | |
| Screen time | |||||
| <5 h | Ref | Ref | |||
| ≥5 h | 0.98 (0.64–1.51) | 0.933 | 0.94 (0.74–1.19) | 0.596 | |
| Leisure-time physical activity and screen time | |||||
| ≥750 MET·min/week and <5 h | Ref | Ref | |||
| ≥750 MET·min/week and ≥5 h | 0.84 (0.41–1.72) | 0.618 | 0.78 (0.55–1.11) | 0.161 | |
| <750 MET·min/week and <5 h | 0.90 (0.56–1.44) | 0.648 | 0.86 (0.68–1.09) | 0.220 | |
| <750 MET·min/week and ≥5 h | 0.98 (0.57–1.67) | 0.927 | 0.86 (0.62–1.20) | 0.370 | |
| (2) Urgency UI | Leisure-time physical activity | ||||
| <750 MET·min/week | Ref | Ref | |||
| ≥750 MET·min/week | 0.77 (0.50–1.18) | 0.226 | 0.95 (0.71–1.27) | 0.720 | |
| Screen time | |||||
| <5 h | Ref | Ref | |||
| ≥5 h | 1.31 (0.91–1.88) | 0.137 | 1.24 (0.98–1.56) | 0.071 | |
| Leisure-time physical activity and screen time | |||||
| ≥750 MET·min/week and <5 h | Ref | Ref | |||
| ≥750 MET·min/week and ≥5 h | 1.17 (0.49–2.78) | 0.723 | 1.26 (0.73–2.17) | 0.390 | |
| <750 MET·min/week and <5 h | 1.23 (0.72–2.11) | 0.442 | 1.04 (0.76–1.42) | 0.794 | |
| <750 MET·min/week and ≥5 h | 1.67 (1.05–2.68) | 0.032 | 1.28 (0.85–1.93) | 0.237 | |
| (3) Mixed UI | Leisure-time physical activity | ||||
| <750 MET·min/week | Ref | Ref | |||
| ≥750 MET·min/week | 0.58 (0.35–0.96) | 0.036 | 0.67 (0.51–0.87) | 0.004 | |
| Screen time | |||||
| <5 h | Ref | Ref | |||
| ≥5 h | 1.00 (0.65–1.53) | 0.987 | 1.27 (0.99–1.62) | 0.059 | |
| Leisure-time physical activity and screen time | |||||
| ≥750 MET·min/week and <5 h | Ref | Ref | |||
| ≥750 MET·min/week and ≥5 h | 0.63 (0.23–1.72) | 0.361 | 1.33 (0.67–2.64) | 0.409 | |
| <750 MET·min/week and <5 h | 1.54 (0.83–2.85) | 0.167 | 1.50 (1.05–2.14) | 0.028 | |
| <750 MET·min/week and ≥5 h | 1.75 (1.01–3.04) | 0.045 | 1.82 (1.20–2.76) | 0.006 | |
| Outcomes . | Variables . | BMI: <25 kg/m2 . | BMI: ≥25 kg/m2 . | ||
|---|---|---|---|---|---|
| OR (95% CI) . | p value . | OR (95% CI) . | p value . | ||
| (1) Stress UI | Leisure-time physical activity | ||||
| <750 MET·min/week | Ref | Ref | |||
| ≥750 MET·min/week | 1.06 (0.69–1.62) | 0.801 | 1.09 (0.88–1.36) | 0.407 | |
| Screen time | |||||
| <5 h | Ref | Ref | |||
| ≥5 h | 0.98 (0.64–1.51) | 0.933 | 0.94 (0.74–1.19) | 0.596 | |
| Leisure-time physical activity and screen time | |||||
| ≥750 MET·min/week and <5 h | Ref | Ref | |||
| ≥750 MET·min/week and ≥5 h | 0.84 (0.41–1.72) | 0.618 | 0.78 (0.55–1.11) | 0.161 | |
| <750 MET·min/week and <5 h | 0.90 (0.56–1.44) | 0.648 | 0.86 (0.68–1.09) | 0.220 | |
| <750 MET·min/week and ≥5 h | 0.98 (0.57–1.67) | 0.927 | 0.86 (0.62–1.20) | 0.370 | |
| (2) Urgency UI | Leisure-time physical activity | ||||
| <750 MET·min/week | Ref | Ref | |||
| ≥750 MET·min/week | 0.77 (0.50–1.18) | 0.226 | 0.95 (0.71–1.27) | 0.720 | |
| Screen time | |||||
| <5 h | Ref | Ref | |||
| ≥5 h | 1.31 (0.91–1.88) | 0.137 | 1.24 (0.98–1.56) | 0.071 | |
| Leisure-time physical activity and screen time | |||||
| ≥750 MET·min/week and <5 h | Ref | Ref | |||
| ≥750 MET·min/week and ≥5 h | 1.17 (0.49–2.78) | 0.723 | 1.26 (0.73–2.17) | 0.390 | |
| <750 MET·min/week and <5 h | 1.23 (0.72–2.11) | 0.442 | 1.04 (0.76–1.42) | 0.794 | |
| <750 MET·min/week and ≥5 h | 1.67 (1.05–2.68) | 0.032 | 1.28 (0.85–1.93) | 0.237 | |
| (3) Mixed UI | Leisure-time physical activity | ||||
| <750 MET·min/week | Ref | Ref | |||
| ≥750 MET·min/week | 0.58 (0.35–0.96) | 0.036 | 0.67 (0.51–0.87) | 0.004 | |
| Screen time | |||||
| <5 h | Ref | Ref | |||
| ≥5 h | 1.00 (0.65–1.53) | 0.987 | 1.27 (0.99–1.62) | 0.059 | |
| Leisure-time physical activity and screen time | |||||
| ≥750 MET·min/week and <5 h | Ref | Ref | |||
| ≥750 MET·min/week and ≥5 h | 0.63 (0.23–1.72) | 0.361 | 1.33 (0.67–2.64) | 0.409 | |
| <750 MET·min/week and <5 h | 1.54 (0.83–2.85) | 0.167 | 1.50 (1.05–2.14) | 0.028 | |
| <750 MET·min/week and ≥5 h | 1.75 (1.01–3.04) | 0.045 | 1.82 (1.20–2.76) | 0.006 | |
UI, urinary incontinence; MET, metabolic equivalent; OR, odds ratio; CI, confidence interval.
(1) Adjusted for age, race, drink status, smoking status, transportation physical activity, menopausal status, hypertension, diabetes, dyslipidemia, cardiovascular disease, pelvic infection, use of female hormones, muscle relaxant, vaginal deliveries, cesarean deliveries, prior hysterectomy, caffeine, and tried to lose weight.
(2) Age, smoking status, transportation physical activity, menopausal status, hypertension, diabetes, dyslipidemia, cardiovascular disease, pelvic infection, use of female hormones, diuretic, vaginal deliveries, cesarean deliveries, prior hysterectomy, and tried to lose weight.
(3) Age, race, drink status, smoking status, menopausal status, hypertension, diabetes, dyslipidemia, cardiovascular disease, pelvic infection, use of female hormones, diuretic, muscle relaxant, vaginal deliveries, cesarean deliveries, prior hysterectomy, caffeine, tried to lose weight and moisture.
Discussion
In the study of the NHANES 2011–2016 sample, we observed an inverse association between leisure-time physical activity and the likelihood of mixed UI among females. Additionally, there was a positive correlation between sedentary behavior and female urgency UI. Notably, brief periods of leisure-time physical activity and prolonged sedentary behavior exhibited a joint effect for the likelihood of urgency and mixed UI among females.
Previous studies have reported certain health problems associated with leisure-time physical activity and sedentary behavior [18, 19]. However, to the best of our knowledge, this study is the first to investigate the independent and combined effects of leisure-time physical activity and sedentary behavior on different subtypes of UI risk among females. UI can result in enduring physical and psychological distress for patients, with varying degrees of impact observed across different subtypes of UI [20]. In a study from China, women pointed out that the severity of mixed UI surpasses that of stress UI and urgency UI, and the overall health burden (including mental health) experienced by patients with mixed UI exceeds that of those with stress UI and urgency UI [21]. The selection of treatment options varies clinically based on the subtype of UI. Thus, it makes sense to focus on different subtypes of UI. For the current study, sedentary behavior only was observed to be linked with female urgency UI, which is consistent with previous research finding [22]. Unlike stress UI, urgency UI is characterized by the involuntary loss of urine accompanied by a sudden and strong urge to urinate, which is recognized as a neurological disorder [23]. Urgency UI is a common symptom of overactive bladder, and inflammation plays a key role in the pathogenesis of overactive bladder [24]. Sedentary behavior increases the production and accumulation of reactive oxygen species, leading to cytokine release and inflammatory markers that ultimately result in endothelial dysfunction [11, 25]. Also, prolonged sitting was also a risk factor for metabolic syndromes which may affect the bladder by impacting the metabolically active urothelium [26]. As Kim MM’s research pointed out, there was an association between moderate physical activity and a reduced likelihood of mixed UI in women. This relationship may be due to the fact that moderate physical activity improves pelvic floor strength and has an effect on neurophysiological mediators involved in the pathogenesis of UI [27]. Our result also found similar result.
Importantly, in this study, subjects with different levels of leisure-time physical activity and screen time (sedentary behavior) were divided into four lifestyle groups to investigate the combined effects of physical activity and sedentary behavior on UI. It showed that the combination of leisure-time physical activity <750 MET·min/week and screen time ≥5 h/day was related to urgency and mixed UI. The effect size of screen time ≥5 h/day on urgency UI was 1.31. When combined with leisure-time physical activity <750 MET·min/week, the effect size increased to 1.53. In other words, the combination of screen time ≥5 h/day and leisure-time physical activity <750 MET·min/week may pose a higher risk for urgency UI than screen time ≥5 h/day alone. These results also suggested a joint effect of brief periods of leisure-time physical activity and prolonged sedentary behavior on the likelihood of urgency and mixed UI. It is worth mentioning that the result of subgroup analysis indicated that increasing the duration of leisure-time physical activity or reducing sedentary behavior appropriately may be advantageous in mitigating the risk of mixed UI, regardless of the individual’s weight status.
This study has important public health implications for female UI prevention. For adult women in the USA, concurrent promotion of leisure-time physical activity and reduction of sedentary behavior should be encouraged to optimize the effectiveness of UI prevention. However, there are also some limitations in this study. First, this cross-sectional study limits the ability to elucidate a causal relationship between leisure-time physical activity, sedentary behavior, and UI. Second, although NHANES data collection adhered to standardized procedures for ensuring data quality, the acquisition of leisure-time physical activity, sedentary behavior, and UI relied on self-reporting, inevitably resulting in some degree of recall bias. Third, multiple confounding factors were adjusted in this study, but it is important to acknowledge that the influence of other confounding factors cannot be entirely eradicated. Hence, a cautious is required when interpreting the results. Future research should consider conducting multicenter prospective clinical trials to better assess the independent and joint effects of leisure-time physical activity and sedentary behavior with the female UI risk.
Conclusion
Our study found an inverse association between leisure-time physical activity and the likelihood of mixed UI among females, and there was a positive correlation between sedentary behavior and female urgency UI. In addition, a lower level of leisure-time physical activity incorporated with prolonged time sedentary behavior was positively related to urgency and mixed UI in a representative sample of the US women, which meant that participants experiencing a lower level of leisure-time physical activity and a higher level of sedentary behavior together might enhance the urgency and mixed UI risk.
Statement of Ethics
The requirement of ethical approval for this was waived by the Institutional Review Board of Wuhan Children’s Hospital (Wuhan Maternal and Child Healthcare Hospital), Tongji Medical College, Huazhong University of Science and Technology because the data were accessed from NHANES (a publicly available database). The need for written informed consent was waived by the Institutional Review Board of Wuhan Children’s Hospital (Wuhan Maternal and Child Healthcare Hospital), Tongji Medical College, Huazhong University of Science and Technology due to retrospective nature of the study.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
No research funding was received.
Author Contributions
C.S. and Z.D. designed the study and collected, analyzed, and interpreted the data. C.S. wrote the manuscript. Z.D. critically reviewed, edited, and approved the manuscript. All authors read and approved the final manuscript.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available in the NHANES database, https://wwwn.cdc.gov/nchs/nhanes/. Further inquiries can be directed to the corresponding author.