Abstract
Introduction: Postoperative hypertension resolution among patients with adrenal incidentalomas and normal hormone levels was unknown. Identifying the predictive factors was beneficial to the management of adrenal incidentalomas. Methods: We conducted a retrospective cohort study, recruiting patients undergoing laparoscopic adrenal tumor resection for adrenal incidentaloma with hypertension and normal hormone levels. Demographic, clinical, treatment, and laboratory data were collected and compared. We used univariable and multivariable logistic regression methods to identify the predictive factors of postoperative hypertension resolution. Results: Of the 171 patients in our study, 130 (76.0%) patients performed a resolution of hypertension, and 57 (33.3%) patients had a significant reduction. Multivariate logistic regression analysis showed that the male sex (odds ratio (OR) 0.305, 95% confidence interval (CI): 0.098–0.948, p = 0.040), body mass index (BMI) (OR 0.973, 95% CI: 0.670–0.938, p = 0.007), aldosterone and plasma renin activity ratio (APR) in erect position (OR 1.206, 95% CI: 1.042–1.397, p = 0.012), and preoperative systolic pressure (OR 1.044, 95% CI: 1.009–1.080, p = 0.014), were significantly associated with the outcomes of hypertension resolution. Discussion/Conclusion: Adrenal incidentalomas patients with hypertension and normal hormone levels would perform hypertension resolution after laparoscopic adrenal tumor resection, especially for females with low BMI, high preoperative systolic blood pressure, and high APR (erect position).
Introduction
Adrenal incidentalomas (AIs) are the most common adrenal gland diseases, which are harmful to health mainly by regulating hormone secretion and substance metabolism [1, 2]. For patients diagnosed with AIs (<4 cm) with normal hormone levels, follow-up observation is usually recommended, remaining a small part received surgical treatment [1]. The long-term sequelae of untreated hypertension have been extensively reported, including potentially irreversible cardiovascular and renal damage. During the follow-up of patients with AIs in our tertiary care center, whether hypertension could be cured by surgical treatment was the primary concern of most patients. Interestingly, we note the varying degrees of reduction in blood pressure (BP) among these patients after surgical treatment.
Based on preoperative clinical variables, several models have been described to predict hypertension resolution, in which aldosterone-producing adenoma patients are most likely to be cured of their hypertension after adrenalectomy [3‒6]. Nevertheless, all the data sets included only adult aldosterone-producing adenoma patients who underwent adrenalectomy, and the potential relationship between hypertension and AIs has been neglected. Herein, we conducted a retrospective cohort study of patients undergoing laparoscopic adrenal tumor resection for AIs with hypertension and normal hormone levels to identify predictive factors of hypertension resolution.
Methods
Study Design and Participants
We designed a retrospective cohort study. The electronic database of the Tongji Hospital, Tongji Medical College, was queried. A total of 2,211 patients with adrenal masses were diagnosed by CT/MRI scans between May 2005 and April 2018. Patients with nonsurgical treatment (n = 384), adrenal malignancy (n = 48) and incomplete medical records (n = 155) were excluded. Patients with bilateral adrenal masses (n = 9), aldosterone and plasma renin activity ratio (APR) > 30 (n = 510), plasma cortisol >22.4 μg/dL (n = 71), positive 24 h urinary catecholamines and their metabolites (n = 18) and those lacking all the above three tests (n = 412) were excluded. Finally, 171 AIs patients with hypertension and normal hormone levels were enrolled in the study (Fig. 1).
These patients requested surgical treatment and signed informed consent for surgery. All patients underwent laparoscopic adrenal tumor resection, precisely removing the hyperplastic gland or mass and preserving normal adrenal tissue. All surgical operations were carried out in our tertiary care center by 2–3 experienced urologists, and the surgeons were senior physicians with a cumulative volume of more than 200 completed laparoscopic adrenalectomy [7].
Variables and Definitions
Baseline clinical characteristics were collected, including age, sex, body mass index (BMI), smoking history, drinking history, history of diabetes, history of the cardia-cerebrovascular disease, preoperative BP, hormone testing results, biochemical results, and tumor characteristics. Intraoperative and postoperative clinical indicators were reviewed, including intraoperative BP variables, operation time, estimated blood loss, postoperative BP, postoperative hospital stay, total expense, and histology. The dosage of antihypertensive drugs was recorded at admission and discharge to the hospital.
Hypertension was defined as systolic BP (SBP) ≥140 mm Hg or diastolic BP (DBP) ≥90 mm Hg [8]. Hypertension grade was defined as follows: (i) Grade 0: SBP <140 mm Hg and DBP <90 mm Hg; (ii) Grade 1: SBP = 140–159 mm Hg and/or DBP = 90–99 mm Hg; (iii) Grade 2: SBP = 160–179 mm Hg and/or DBP = 100–109 mm Hg; and (iv) Grade 3: SBP ≥180 mm Hg or DBP ≥110 mm Hg. Average SBP and DBP were calculated from multiple measurements. Hypertension resolution in these patients was defined as (i) postoperative BP decline to normal levels (<140/90 mm Hg) or (ii) doses of antihypertensive medication after laparoscopic adrenal tumor resection were reduced. Here, patients with a decline of SBP of more than 20 mm Hg after surgical resection were further classified as the significant reduction group [9].
Exploring the Clinical Characteristics of the Patients with Reduction of BP
The perioperative variables between the persistent hypertension group and the resolution group were compared. The statistically significant variables in comparing the two groups or reported to be significant based on the previous literature were first analyzed by univariable logistic regression and further explored by multivariate logistic regression analysis [10]. A nomogram was created using the R statistical software (the “rms” package), and the area under the curve was calculated.
Statistical Analysis
Continuous, normally distributed variables were described as the mean (standard deviation, min, max) and compared by the t test or paired t test; non-normally distributed variables were described as the median (interquartile range) and compared with the Wilcoxon rank-sum test. Categorical data were presented as frequencies (%) and compared using the χ2 test. SPSS 21.0 (IBM Corporation, Armonk, NY, USA) and R statistical package (v.3.5.2; R Foundation for Statistical Computing, Vienna, Austria; https://www.r-project.org) were used for all statistical analysis. A two-sided p < 0.05 was considered to be statistically significant.
Results
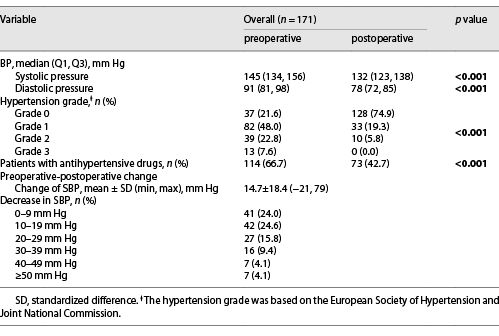
Variation of Blood Pressure and Antihypertensive Drugs
Preoperative SBP and DBP were 145 (134, 156) and 91 (81, 98) mm Hg, respectively. Meanwhile, postoperative SBP and DBP were 132 (123, 138) and 78 (72, 85) mm Hg, respectively, which were significantly reduced (p < 0.001 and p < 0.001, respectively). The hypertension grade and the number of patients treated with antihypertensive drugs were significantly reduced after the surgery (p < 0.001 and p = 0.001, respectively). The decreased value of SBP was 14.7 ± 18.4 mm Hg. A decline of postoperative SBP by 0–9 mm Hg, 10–19 mm Hg, 20–29 mm Hg, 30–39 mm Hg, 40–49 mm Hg and >50 mm Hg was observed in 41 (24.0%), 42 (24.6%), 27 (15.8%), 16 (9.4%), 7 (4.1%), and 7 (4.1%) patients, respectively (Table 1; Fig. 2).
Outcomes of the BP and antihypertensive drugs of the patients. a Perioperative BP changes of the overall patients, n= 171. b Proportion of patients taking hypertension drugs during the perioperative period, n= 171.
Outcomes of the BP and antihypertensive drugs of the patients. a Perioperative BP changes of the overall patients, n= 171. b Proportion of patients taking hypertension drugs during the perioperative period, n= 171.
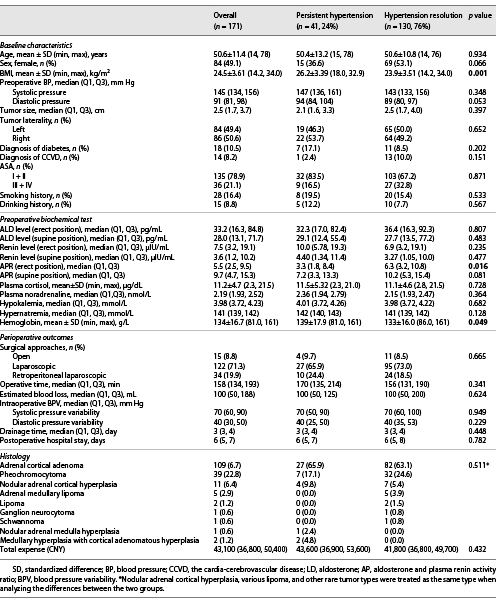
Baseline Characteristics and Preoperative Biochemical Test of Patients
Of the 171 patients treated with laparoscopic adrenal tumor resection, 130 (76.0%) and 41 (24%) were included in the hypertension resolution and persistent hypertension groups. In comparison with those in the hypertension resolution group, a higher BMI (26.2 ± 3.39 vs 23.9 ± 3.51 kg/m2, p = 0.001) and a lower APR (erect position) (3.3 [1.8, 8.4] vs. 6.3 [3.2, 10.8], p = 0.016) were detected in the persistent hypertension group. A significant increase in hemoglobin levels was found in the persistent hypertension group (p = 0.049) (Table 2).
According to the decreased magnitude of SBP, patients in the hypertension resolution group were further divided into a significant reduction group (n = 57, 33.3%) and the general reduction group (n = 73, 42.7%). Lower BMI (26.2 ± 3.39 vs. 23.6 ± 3.44 kg/m2, p < 0.001), renin levels (erect position, 10.0 [5.78, 19.3] vs. 4.96 [2.11, 10.9] µIU/mL, p = 0.024), and hemoglobin (139 ± 17.9 vs. 131 ± 16.9 g/L, p = 0.010) were detected in significant reduction group than those of the persistent hypertension group. Some of the variables in the significant reduction group were higher, such as sex ratio (female, 15 [36.6%] vs. 36 [63.2%], p = 0.017), preoperative SBP (147 [136, 161] vs. 156 [148, 164] mm Hg, p = 0.007), APR (erect position, 3.3 [1.8, 8.4] vs. 8.20 [4.70, 12.6], p < 0.001), and APR (supine position, 7.65 [3.38, 13.3] vs. 11.6 [7.28, 16.6], p = 0.014) (online suppl. Table s1; for all online suppl. material, see www.karger.com/doi/10.1159/000524803).
Factors Associated with Hypertension Resolution
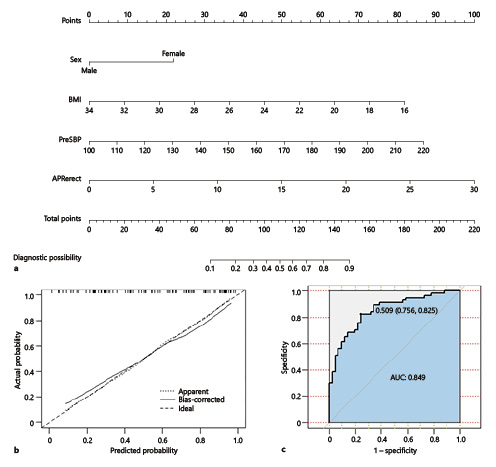
Univariate logistic regression analysis screened out the factors: sex, BMI, preoperative SBP, hemoglobin, and APR (erect position). Multivariate logistic regression analysis showed that male sex (odds ratio (OR) 0.305, p = 0.040), BMI (OR 0.793, p = 0.007), preoperative SBP (OR 1.044, p = 0.016), and APR (erect position; OR 1.206, p = 0.012) were significantly associated with resolution of hypertension (Table 3).
A nomogram that incorporated the four significant risk factors was constructed. The total score of each patient was calculated based on sex, BMI, preoperative SBP, and APR (erect position) to estimate the probability of the improvement of postoperative hypertension (Fig. 3a). The calibration curve of the nomogram was presented in Figure 3b, in which the two curves fitted well. The two curves represented the predicted probability of improving postoperative hypertension, indicating that the nomogram showed robust discrimination. By analyzing the receiver operating characteristic curve (Fig. 3c), the area under the curve was calculated as 0.849 (95% confidence interval: 0.806–0.894). When the probability value was 0.509, the sensitivity and specificity of the predicted results were optimal.
Nomogram, calibration of the nomogram for anastomotic leakage, and the receiver operating characteristic curve. The nomogram was created using the R statistical software (the “rms” package). a Draw a line perpendicular to the corresponding axis of each risk factor until it reaches the top line labeled “Points.” Sum up the number of points for all risk factors, then draw a line descending from the axis labeled “Total Points” until it intercepts the “Probability.” b The x-axis shows the predicted probability of significant improvement of hypertension, and the y-axis shows the observed probability of significant improvement of hypertension. The apparent curve coincided well with the ideal curve. c The AUC was calculated as 0.849 (95% CI: 0.806–0.894). AUC, area under the curve.
Nomogram, calibration of the nomogram for anastomotic leakage, and the receiver operating characteristic curve. The nomogram was created using the R statistical software (the “rms” package). a Draw a line perpendicular to the corresponding axis of each risk factor until it reaches the top line labeled “Points.” Sum up the number of points for all risk factors, then draw a line descending from the axis labeled “Total Points” until it intercepts the “Probability.” b The x-axis shows the predicted probability of significant improvement of hypertension, and the y-axis shows the observed probability of significant improvement of hypertension. The apparent curve coincided well with the ideal curve. c The AUC was calculated as 0.849 (95% CI: 0.806–0.894). AUC, area under the curve.
Discussion
Therapeutic strategies for AIs patients with normal hormone levels were conservative. It is recommended against performing surgery in patients with an asymptomatic, nonfunctioning unilateral adrenal mass and obvious benign features on imaging studies [1, 11]. In relevant studies, after surgical resection, hypertension resolution in patients diagnosed with primary aldosteronism is 42–84% [12‒14], and the rate of hypertension resolution in patients diagnosed with Cushing’s syndrome is about 39–87% [15‒17]. According to our study, 130 patients (76.0%) performed the resolution of hypertension, and 57 patients (33.3%) significantly reduced BP. The hypertension grade and the rate of treatment with antihypertensive drugs were also significantly reduced. Notably, this study indicated that AIs patients with normal hormone levels could benefit from surgical treatment.
Several models have been described to predict the resolution of hypertension. The Wachtel et al. [4] scoring system was created based on a single American tertiary hospital center data set. The authors determined that female sex, BMI ≤25 kg/m2, duration of hypertension <5 years, serum creatinine ≤0.8 mg/dL, and <2 preoperative antihypertensive medications were the most critical factors in terms of long-term BP control [4]. Utsumi et al. [5] used a multi-institutional data set of Japanese patients to construct a nomogram. They used multivariate logistic regression analysis to identify predictors, such as age, duration of hypertension, and the number of antihypertension drug classes [5]. Zarnegar et al. [6] constructed a predictive logistic regression model based on two databases from the USA. A total of four factors were identified: female sex, duration of hypertension ≤6 years, BMI ≤25 kg/m2, and two or fewer antihypertensive medications [6]. Multivariate logistic regression analysis showed that male sex, BMI, preoperative SBP, and APR (erect position) were significantly associated with reducing BP in our study. A nomogram model was also established to predict the resolution of hypertension based on multivariate logistic regression analysis. Our results were close to the results of the three clinical trials and could be considered an essential addition to the models predicting the resolution of hypertension. The nomogram model shows promising clinical applicability, which can screen appropriate patients for surgery from AIs patients with normal hormone levels.
By comparing the clinical data of the hypertension resolution group and the persistent hypertension group, we noted higher BMI and lower APR (erect position) in the persistent hypertension group. It is well known that a high BMI is a typical signal in patients with hypertension [18‒20]. Patients in the hypertension resolution group have higher APR (erect position), which indicates that hypertension might be related to aldosterone secretion from the adrenal mass. Primary aldosteronism has emerged as one of the most common correctable causes of secondary hypertension, with prevalence ranging from 6% to 20% in the hypertensive population [21], and unilateral laparoscopic adrenal tumor resection is the treatment for patients.
Our study has several limitations. The sample size of eligible cases was small, and the nomogram model has not been validated against other large sample databases. Since the retrospective study design, not all needed laboratory findings were collected, such as ethnic background, family history of hypertension, pathological results, etc. Therefore, their role might be undervalued. We lack the long-term follow-up outcomes of the patients. So, the findings of this study should be interpreted as exploratory and descriptive. A multicenter, large sample size, and prospective study will be required. However, such patients are rare, and the results are somewhat interpretable, so we present the study results.
Conclusion
We first reported that hypertension is effectively resolved for AIs patients with normal hormone levels after laparoscopic adrenal tumor resection, especially for females with low BMI, high preoperative SBP, and high APR (erect position). Our research is based on single-center data, which needs to be verified by external data.
Acknowledgment
We thank the Department of Medical Records of Tongji Hospital for providing the original data.
Statement of Ethics
The study was performed following the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The study has been granted an exemption from requiring ethics approval from the Ethical Committee of Tongji Hospital for its respective observational design. No human participants were involved. The data collected was through the digitized medical records system, with permission from the Medical Records Department. All personally identifiable information was deleted during the data analysis and the manuscript.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
This study was supported by grants from the National Natural Science Foundation of China (NSFC #82070715, #31570988) and the Natural Science Foundation of Hubei Province (#2021CFB419). Funding sources were not involved in preparing materials or manuscripts.
Author Contributions
Jing Wang and Yunpeng Zhu: project development, data collection, data analysis, and manuscript writing. Zhixian Wang and Chang Liu: protocol/project development and data analysis. Shiliang Liu and Xing Li: data collection and management; Ruibao Chen, Ying Zhan Shaogang Wang, and Xiaoyong Zeng: manuscript editing and revision for important intellectual content.
Data Availability Statement
All data generated or analyzed during this study are included in this article and its online supplementary material. According to the request from the Ethical Committee of Tongji Hospital, the data is not openly available. Further inquiries can be directed to the corresponding author (Prof. Xiaoyong Zeng, [email protected]).