Abstract
Introduction: Robot-assisted partial nephrectomy (RAPN) has been increasingly used for renal cell carcinoma in recent years. But the advantages of RARN over open partial nephrectomy (OPN) are still controversial. Methods: We searched the articles between 1997 and 2021 in PubMed, Web of Science, Cochrane Library, and EMbase databases. The parameters were perioperative outcomes including operating time (OT), warm ischemic time (WIT), estimated blood loss (EBL), positive surgical margin (PSM), preoperative and postoperative estimated glomerular filtration rate (eGFR), length of stay (LOS), and intraoperative and postoperative complications. Stata 13.0 software was used for the meta-analysis. Results: Seven studies with 2,646 patients (1,285 in RAPN vs. 1,361 in OPN) were included in the analysis. There were no significant differences in OT (WMD [95% confidence interval (CI)]: 0.14 [−0.33, 0.61], p = 0.570); WIT (WMD [95% CI]:0.28 [−0.13, 0.69], p = 0.187); PSM (odds ratio [OR] [95% CI]: 1.04 [0.37, 2.94], p = 0.944); preoperative eGFR (OR [95% CI]: 0.11 [−0.01, 0.23], p = 0.071); postoperative eGFR (OR [95% CI]: −0.11 [0.27, 0.04], p = 0.159); and intraoperative complications (OR [95% CI]: 0.13 [0.02, 1.04], p = 0.055) between 2 groups. But there were still less EBL (WMD [95% CI]: −0.67 [−1.07, −0.28], p = 0.001), shorter LOS (WMD [95% CI]: −1.09 [−1.86, −0.32], p = 0.005) and fewer postoperative complications (OR [95% CI]: 0.51 [0.38, 0.68], p = 0.000). Conclusions: Compared with OPN, RAPN appears to achieve partly similar short-term functional outcomes. Meanwhile, some results are inconsistent with previous studies which seem to show that tumor type is also an important factor in comparison between RAPN and OPN, but the analysis is not carried out due to lack of complete data. Therefore, more high-quality random controlled trials are acquired.
Introduction
Renal cell carcinoma (RCC) is the third most common urological cancer, and its incidence and detection rate have been increasing with the improvement and wide application of diagnostic tools in recent years [1, 2]. Although new therapies have been developed, partial nephrectomy (PN) is still the “gold standard” for the localized cT1 RCCs [3]. However, PN is not fully utilized compared with radical nephrectomy (RN) [4, 5], although PN has been proven to be equivalent to RN in oncology for small renal masses [6]. In addition, the standard operation approach for PN is also disputed [7, 8]. The one of possible reasons is relevant learning curve. For instance, laparoscopic PN has a steep learning curve, which restricts the use of urologists [9]. But the emergence of robot-assisted PN (RAPN) apparently reduced the learning curve [10, 11].
Previously, compared with laparoscopic PN, many studies have already verified the significant advantages of RAPN [10, 11]. On the other hand, a meta-analysis also confirmed that RAPN appears to have lower morbidity and achieves similar short-term functional outcomes compared with open PN (OPN), but research objects are not limited to RCC patients [12]. Interestingly, a current meta-analysis has shown that RARN is not superior to LRN in patients with RCC in terms of perioperative outcomes [13]. Considering this situation, we aim to determine which surgical method is more suitable for patients with cT1 RCC through meta-analysis and systematic review.
Materials and Methods
Search Strategy
This systematic review and meta-analysis were performed in adherence to Preferred Reporting Items for Systematic Reviews and Meta-Analysis criteria [14]. We used the search terms: “robot-assisted” OR “robotic-assisted” OR “robotic” OR “robot” OR “open”OR “partial nephrectomy” OR “renal cell carcinoma,” and searched the articles which published between 1997 and 2021 in PubMed, Web of Science, Cochrane Library, and EMbase databases. The search was limited to publish in English. Two authors independently evaluated each included study and any differences or debates were resolved by consensus.
Inclusion/Exclusion Criteria
Studies were included if they satisfied 4 criteria: (1) study type was randomized controlled trial, cohort study, or case-control study; (2) studies performed in adults diagnosed with T1 RCC; (3) studies comparing RAPN with OPN; and (4) at least, evaluation of one of the perioperative outcomes such as operative time (OT), warm ischemic time (WIT), estimated blood loss (EBL), postoperative length of hospital stay (LOS), preoperative estimated glomerular filtration rate (eGFR), postoperative eGFR, positive surgical margin (PSM), intraoperative complications and postoperative complications. Exclusion criteria were as follows: (1) no comparison performed between RAPN and OPN/LRN and OPN; (2) patients with benign and bilateral tumors; (3) patients with solitary kidney; (4) reviews, editorials, letters to editors, comments, case reports, unpublished articles and conference abstracts; and (5) studies with unavailable data.
Data Extraction
Data extraction was conducted independently by 2 authors, and discrepancies were resolved by negotiation. The following data were extracted from each study: first author, year of publication, region, time period of RAPN/OPN, institution, number of surgeons, study design, number of patients, age, sex, body mass index, tumor size, clinical stage, pathological stage and outcomes (including OT, WIT, EBL, LOS, preoperative eGFR, postoperative eGFR, PSM, intraoperative complications, and postoperative complications). If continuous variables in the article were expressed as median (interquartile range), it would be converted to mean ± standard deviation [15].
Risk-of-Bias Assessments
The Risk of Bias in Non-Randomized Studies-of Interventions tool [16] was used to evaluate publication bias and assessed this bias according to seven domains: confounding bias, selection bias, bias in measurement classification of interventions, bias due to deviations from intended interventions, bias due to missing data, bias in measurement of outcomes, and bias in selection of the reported result.
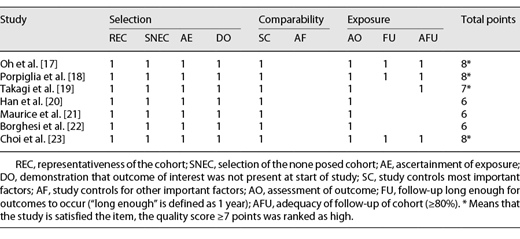
Quality Assessment
All included studies were evaluated using the Newcastle-Ottawa scale [17], and the quality of studies was evaluated by measuring 3 aspects of the study design: patient selection, comparability of the study groups, and assessment of outcomes. Only when the study had a score of ≥6 could it be considered as high quality, otherwise, the study was indicated as low quality.
Statistical Analysis
The meta-analysis was performed on Stata v.13.0 software (Stata Corp, College Station, TX, USA). Dichotomous and continuous variables were pooled as weighted mean difference (WMD) and odds ratio (OR), respectively. 95% Confidence intervals (CIs) were used to assess all data. The degree of heterogeneity was measured by the I2 statistic, when I2 > 50%, heterogeneity was considered significant statistically. The data were analyzed by a random-effect model; otherwise, a fixed-effects model was used. All statistical tests were performed two-sided, and p ≤ 0.05 was considered statistically significant. Subgroup analysis was also carried out according to study design, setting, number of sample, and region. Sensitivity analysis was performed by omitting individual studies one by one for some outcomes such as OT, WIT, EBL, and LOS. Since there were less than 10 studies in this meta-analysis, funnel plot was not used to assess publication bias.
Results
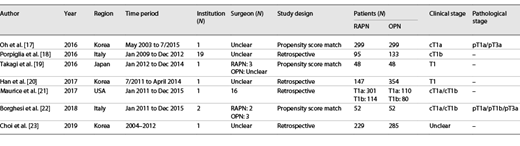
Study Characteristics
As shown in Figure 1, 7 eligible studies were finally included with a total of 2,646 patients (1,285 patients in the RAPN and 1,361 in OPN) [17-23]. Among the 7 studies, there were 3 propensity score matched [17, 19, 22] and 4 retrospective studies [18, 20, 21, 23]. Five studies were single-center [17, 19-21, 23] and 2 studies were multicenter [18, 22]. It is pity that no studies were single surgeon and most of them were unclear. All the studies mentioned clinical stage except for one study [23]. Among them, 2 studies [17, 18] included only cT1a and cT1b RCC patients, respectively. The clinical stage of RCC patients in 2 studies [19, 20] was not provided in detail. The 2 studies [21, 22] included cT1a and cT1b RCC patients, but one of them separated the 2 populations [21], and the other was the opposite [22]. In addition, pathological stage was performed in only 2 studies [17, 22]. The characteristics of included studies were presented in Table 1, and the quality assessment of included studies was presented in Table 2.
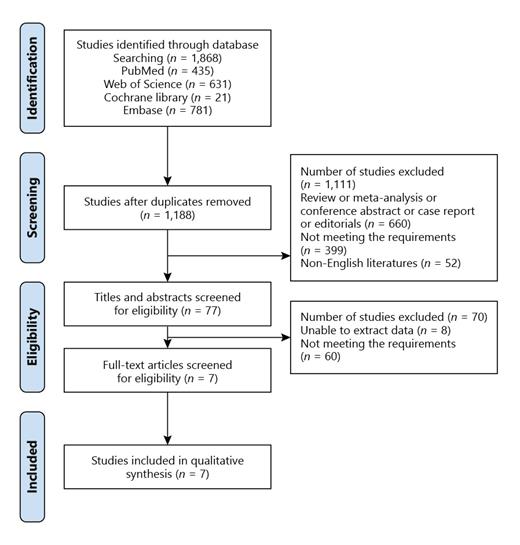
Systematic reviews and meta-analysis flow diagram of studies identified, included and excluded.
Systematic reviews and meta-analysis flow diagram of studies identified, included and excluded.
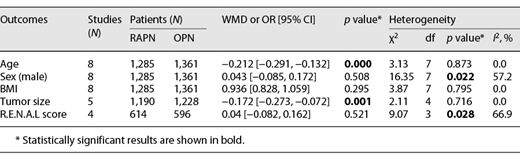
Demographics and Tumor Characteristics Variable
As shown in Table 3 and online supplementary Figure S1 (see www.karger.com/doi/10.1159/000521881 for all online suppl. material), there were no significant differences between the 2 groups in terms of sex (male: OR [95% CI]: 0.043 [−0.085, 0.172]; p = 0.508), body mass index (WMD [95% CI]: 0.936 [0.828, 1.059]; p = 0.295) and R.E.N.A.L score (WMD [95% CI]: 0.04 [−0.082, 0.162]; p = 0.521), but there were significant differences between the 2 groups in terms of age (WMD [95% CI]: −0.212 [−0.291, −0.132]; p = 0.000) and tumor size (WMD [95% CI]: −0.172 [−0.273, −0.072]; p = 0.001).
Meta-Analysis Results
Operative Time
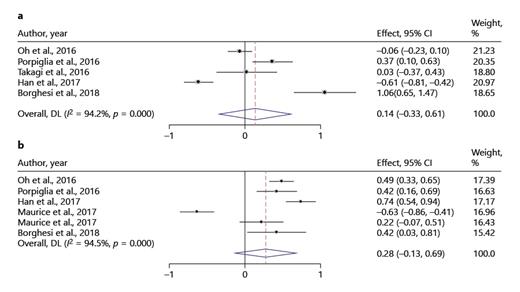
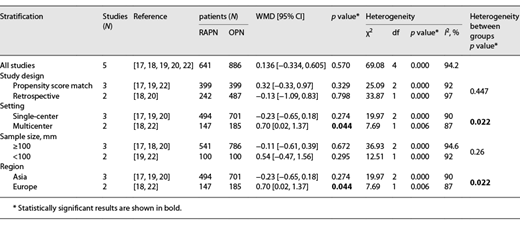
Five studies were included in the analysis of OT, and total of 1,527 patients (641 in RAPN vs. 886 in OPN) [17-20, 22]. A random-effect model was used to analyze the data (I2 = 94.2%). The results indicated no significant differences for OT between RAPN and OPN (WMD [95% CI]: 0.14 [−0.33, 0.61], p = 0.570), although there was a high heterogeneity (Fig. 2a).
Forest plots evaluating the OT and the WIT between RAPN and OPN: the OT (a); WIT (b). Note: weights are from random-effects model.
Forest plots evaluating the OT and the WIT between RAPN and OPN: the OT (a); WIT (b). Note: weights are from random-effects model.
Warm Ischemic Time
The data of WIT were obtained from 5 studies and including 2023 patients (999 in RAPN vs. 1,024 in OPN) [17, 18, 20-22]. There was also no significant difference between RAPN and OPN in the pooled analysis (random-effect model: I2 = 94.5%, WMD [95% CI]: 0.28 [−0.13, 0.69], p = 0.187) (Fig. 2b).
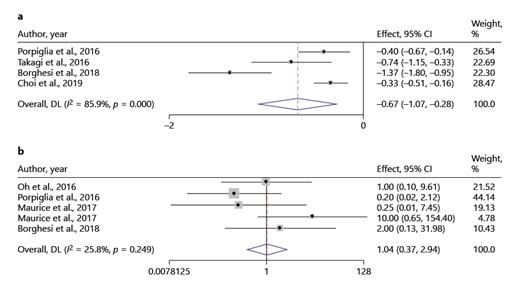
Estimated Blood Loss
Four studies were included in the meta-analysis [18, 19, 22, 23], and totaling 942 patients (RAPN vs. OPN: 424 vs. 518). Due to a great heterogeneity, a random-effect model was used (I2 = 85.9%). The pooled analysis indicated EBL in RAPN was less than that in OPN (WMD [95% CI]: −0.67 [−1.07, −0.28], p = 0.001) (Fig. 3a).
Forest plots of studies evaluating the EBL and the PSM between RAPN and OPN: EBL (a); PSM (b). Note: weights are from random-effects model.
Forest plots of studies evaluating the EBL and the PSM between RAPN and OPN: EBL (a); PSM (b). Note: weights are from random-effects model.
Positive Surgical Margin
1,522 patients were analyzed in 4 studies [17, 18, 21, 22]. PSM was reported in 27/852 of patients who underwent RAPN and 24/670 of patients who underwent OPN. The data showed that RAPN offered a comparable PSM to OPN (fixed effect model: I2 = 25.8%, OR [95% CI]: 1.04 [0.37, 2.94], p = 0.944) (Fig. 3b).
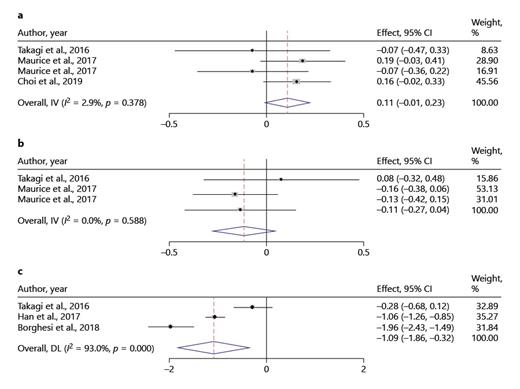
Preoperative and Postoperative Estimated Glomerular Filtration Rate
Three studies were included in the analysis of preoperative eGFR [19, 21, 23], and two were included in the analysis of postoperative eGFR [19, 21]. Among them, a total of 1,215 patients in preoperative eGFR (692 in RAPN vs. 523 in OPN), and a total of 701 patients in postoperative eGFR (463 in RAPN vs. 238 in OPN). The results were similar between the 2 groups, whatever were preoperative eGFR or postoperative eGFR, and low heterogeneity were found in the two eGFRs (preoperative eGFR: fixed effect model: I2 = 2.9%, OR [95% CI]: 0.11 [−0.01, 0.23], p = 0.071; postoperative eGFR: fixed effect model: I2 = 0.0%, OR [95% CI]: −0.11 [0.27, 0.04], p = 0.159) (Fig. 4a–b).
Forest plots of evaluating the preoperative eGFR, postoperative eGFR, and the LOS between RAPN and OPN: preoperative eGFR (a); postoperative eGFR (b); postoperative LOS (c). Note: weights are from random-effects model.
Forest plots of evaluating the preoperative eGFR, postoperative eGFR, and the LOS between RAPN and OPN: preoperative eGFR (a); postoperative eGFR (b); postoperative LOS (c). Note: weights are from random-effects model.
Postoperative Length of Hospital Stay
There were 3 studies were included in reporting LOS, involving 701 patients, of which 247 underwent RAPN and 454 underwent OPN. The data showed that the patients who underwent RAPN had a shorter postoperative LOS than those who underwent OPN (random-effect model: I2 = 93.0%, WMD [95% CI]: −1.09 [−1.86, −0.32], p = 0.005) (Fig. 4c).
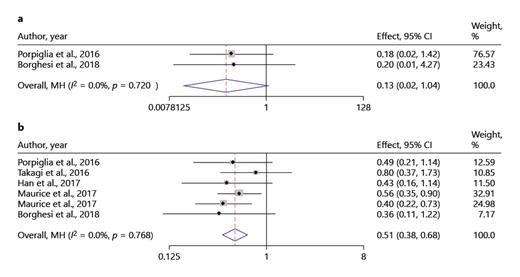
Intraoperative and Postoperative Complications
The illustrations of intraoperative and postoperative complications were set in Figure 5. There was no significant difference in intraoperative complications between the two approaches (fixed effect model: I2 = 0.0%, OR [95% CI]: 0.13 [0.02, 1.04], p = 0.055) (Fig. 5a), but the postoperative complications were dramatically fewer in RAPN compared to OPN (fixed effect model: I2 = 0.0%, OR [95% CI]: 0.51 [0.38, 0.68], p = 0.000) (Fig. 5b).
Forest plots of evaluating the intraoperative and postoperative complications between RAPN and OPN: intraoperative complications (a); postoperative complications (b). Note: weights are from Mantel-Haenszel model.
Forest plots of evaluating the intraoperative and postoperative complications between RAPN and OPN: intraoperative complications (a); postoperative complications (b). Note: weights are from Mantel-Haenszel model.
Subgroup Analysis
Subgroup analysis of OT was shown in Table 4 and online supplementary Figure S2. The findings of no significant difference for OT were consistent in all subgroup analysis except for multicenter and Europe subgroup. Subgroup differences were found in setting and region.
Sensitivity Analysis and Publication Bias
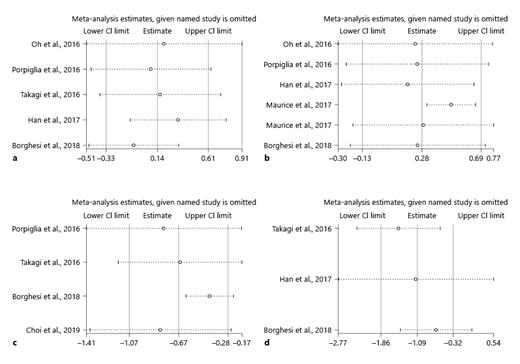
Although the included studies had a high quality (all studies had a 6 score or higher), some parameters such as OT, WIT, EBL, and LOS were still highly heterogeneous. So, it is necessary that a sensitivity analysis was performed to improve the reliability of the analysis of these parameters. Deleting studies one by one to recalculate the combined average difference. After deleting any one study, all new pooled mean differences remained unchanged (Fig. 6). Publication bias was assessed by the Risk of Bias in Non-Randomized Studies-of Interventions tool and suggested that all comparative studies had a moderate risk of bias [17-23].
Sensitivity analysis of studies reporting the 4 perioperative outcomes between RAPN and OPN: OT (a); WIT (b); EBL (c); LOS (d).
Sensitivity analysis of studies reporting the 4 perioperative outcomes between RAPN and OPN: OT (a); WIT (b); EBL (c); LOS (d).
Discussion
Many studies focused on the comparison of perioperative outcomes between RAPN and OPN [17, 19, 22], but there are not restrictions in the tumor types of patients (including malignant tumors (clear cell, papillary, and chromophobe) and benign tumors (angiomyolipoma [AML] and oncocytoma)). To the best of our knowledge, this is the first meta-analysis to report the comparative outcomes of RAPN versus OPN in patients with clinical T1 (cT1) RCC. Currently, several studies suggested that PN is considered as the suitable option for clinical T1 RCC [24-26]. In this study, we indicated that there were no significant differences in terms of OT, WIT, PSM, preoperative eGFR, postoperative eGFR, and intraoperative complications. Hence, RAPN appears to be a safety and effective surgical treatment for patients with cT1 RCC, although only perioperative outcomes were compared in this meta-analysis.
In the meta-analysis conducted by Xia et al. [12], the analysis of pooled data showed that there is a longer OT and WIT in RAPN. Grivas et al. [27] also found the consistent results. However, our analysis found that OT and WIT are no significant difference between the 2 groups. It seemed to indicate that OT and WIT are related to the tumor types of patients. But considering the high heterogeneity (I2 = 94.2%), these results should be interpreted with caution. On the other hand, subgroup analysis showed that OT appears to be also related to the difference from setting and region, and it is interesting that all single-center studies are from Asia and multicenter studies are from Europe. In fact, OT may be related to the technical proficiency and experience of the surgeon, for example, the mean OT of robotic surgery of Takagi et al. [19] is nearly 1 h longer than that of Oh et al. [17]. Similarly, the WIT is related with ability to suture with RAPH, and the WIT of RAPN can be controlled to less than 20 min, if it is operated by an experienced surgeon [10, 18, 28]. Some initial experiences from a few studies which focused on the outcomes of RAPN for T1b renal lesions suggested that a significant higher WIT in T1b to T1a renal tumors [29, 30]. In addition, the EBL and LOS in RAPH were less than that in OPN, which are consistent with previous studies [19, 22].
Our meta-analysis showed similar PSM rate, preoperative eGFR, and postoperative eGFR between RAPN and OPN groups. Although it is still controversial whether PSM will affect the long-term oncology results of patients with RCC, complete removal of the tumor and achieving a negative margin is undoubtedly one of the key goals of PN [31, 32]. In terms of complications, we found that patients undergoing RAPN had a lower rate of postoperative complications, while intraoperative complications had no significance difference between the 2 groups. Similar findings were also supported by the recent meta-analysis [12, 27].
When it comes to some parameters, such as OT and WIT, which were different from the results of previous studies, it is confirmed that tumor types might be an important factor. However, due to lack of complete data in included studies, we could not carry out subgroup analysis of clinical and pathological stages.
In fact, Cacciamani et al. [33] recently report a study protocol about comparing robotic versus open urological oncological surgery, and point out that the comparison between them should focus on five key questions: penetrance in the field, perioperative data, procedural morbidity, oncological outcomes, functional outcomes, and financial cost. But it is regrettable that the outcomes of cost are not offered by included studies. Therefore, in future research, cost is designed as one of the parameters, which can prove more objectively and comprehensively that RAPN is superior to OPN. However, cost variations may depend on the characteristics of the hospital (such as size, geography, teaching status, and profit status) [34, 35], and these potential confounding factors lead to uncertainty in the cost results.
In addition, it is worth noting that age and tumor size had significant differences between the 2 groups. After a series of analyses, we found that patients of RAPN group (mean age ranged from 51.7 to 61.35 years old) were younger than OPN group (mean age ranged from 53.25 to 62.77 years old) and mean tumor size of RAPN group (ranged from 2.5 to 4.96 years old) was smaller than OPN group (ranged from 2.8 to 5 cm). However, it is necessary that demographic data should be as comparable as possible to ensure that the influence of confounding factors on the study was minimized and the results were more reliable. Hence, researchers need to pay more attention to the comparability of demographic data in research design.
However, there are some limitations in the present analysis. First, most of the included studies were the retrospective analysis, and some studies were small sample size. Second, the learning curve of the surgeons was not accounted for before conducting the analyses, and it is worth mentioning that most of the studies declared the surgeons were beyond learning curve. Third, heterogeneities between the studies for OT, WIT, EBL, and LOS were relatively high. The possible explanation is that all of them are continues variables; on the contrary, categorical variables tend to have low heterogeneities. But this cannot explain all the data, after all, the heterogeneity of preoperative eGFR and postoperative eGFR is not high. Fourth, due to incomplete data, it is difficult to get the ASA score with statistical significance so that the quality of meta-analysis was limited. Finally, a cost outcomes was not included due to lack of data. Indeed, cost is the one of main factors which might restrict the application of robotics.
Conclusion
Our meta-analysis suggests that RAPN may be more suitable for the patients with cT1 RCC, as it offers less EBL, shorter LOS, and fewer postoperative complications. Meanwhile, some results are inconsistent with previous studies showing that tumor type may be an important factor in comparison between RAPN and OPN. However, the analysis is not carried out due to lack of complete data. Therefore, random controlled trials with well-designed, large sample size, and long-term fellow-up are still needed, and tumor type should need to be taken into account.
Statement of Ethics
Ethical approval was not required for this study in accordance with local/national guidelines.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
This manuscript did not receive any funding.
Author Contributions
Y.N. planned and designed the research; XY. tested the feasibility of the study; Y.N. wrote the manuscript; all the authors approved the final version of the manuscript.
Data Availability Statement
All data generated or analyzed during this study are included in this. Further enquiries can be directed to the corresponding author.