Abstract
Introduction: In living donor transplantation choosing the right donor and donor side for laparoscopic donor nephrectomy is a challenging task in clinical practice. Knowledge about anomalies in renal blood supply are crucial to evaluate the feasibility of the operative procedure. Few data so far exist whether the existence of a retroaortic left renal vein has an impact on living kidney transplantation outcome for donor and recipient. Materials and Methods: We retrospectively analyzed 221 patients who underwent laparoscopic living donor nephrectomy between 2011 and 2017 for existence of a retroaortic left renal vein. Clinical characteristics and operative outcomes for donors and recipients were analyzed. Results: 221 patients underwent donor nephrectomy between 2011 and 2017; 11 patients (4.98%) showed the feature of a retroaortic left renal vein, and in 8 patients (72.7%) out of those 11 the left kidney was chosen for transplantation. Mean preoperative serum creatinine was 0.77 (0.49–0.98) mg/dL and 1.28 (0.97–1.64) mg/dL at discharge. In recipients mean serum creatinine preoperatively, after 1 week, 1 month,1 year, 2 and 3 years of follow-up was 10.36 (6.09–20.77) mg/dL, 1.71 (0.67–2.72), 1.33 (0.70–1.89), 1.31 (0.95–2.13), 1.31 (0.98–2.13) and 1.33 (1.03–1.84), respectively. Neither donors nor recipients suffered from any operative complications. Conclusions: Laparoscopic living donor nephrectomy of a left kidney with retroaortic renal vein is safe for the donor, without limitation in the outcome for the recipient.
Introduction
Laparoscopic donor nephrectomy has widely been accepted as standard procedure for living donor transplantation. This is due to patients experiencing less postoperative pain, a shorter hospital stay and earlier return to normal activity compared to open donor nephrectomy [1, 2].
Evaluation and identification of the right donor in clinical practice remains a challenging task, including evaluation of operative feasibility of laparoscopic donor nephrectomy. Therefore, anatomical anomalies of renal blood supply play an important role, not only for donor selection, but also for donor anatomical side selection. Renal blood supply varies in number of vascular supply including anatomical course and number of blood vessels present [3]. Data on living donor nephrectomy of kidneys with multiple arteries suggest that there is no higher risk for donor and recipient, although the operative steps are surgically more difficult [4, 5]. However, so far there is only little evidence regarding the consequence of anatomical course anomalies of the renal vein, especially cases with retroaortic left veins. In this analysis, we aim to discuss results of laparoscopic donor nephrectomies in patients with left-sided retroaortic veins.
Materials and Methods
Patients
For the present study all laparoscopic donor nephrectomies performed between 2011 and 2017 at Charité Hospital Berlin, Department for Urology, were analyzed for anatomical variations of the left renal vein. Approval by the Institutional Review Board of Charité Hospital Berlin was not necessary, and the need for informed consent was waived because of this study’s retrospective, noninterventional design and because patient data confidentiality and privacy were maintained.
Patient Preparation
All donors underwent an extensive medical workup to ensure there were no malignancies and chronic diseases. Renal vascular imaging was performed with multislice CT angiography and/or with MR angiography. Donor split renal function was tested using 99mTC-MAG3 renography. In cases of a relevant difference between the left and the right donor kidney, the kidney with inferior function was chosen, regardless of the renal vascular anatomy.
Surgical Technique
Laparoscopic Donor Nephrectomy
For laparoscopic donor nephrectomy, a pure laparoscopic, non-hand-assisted procedure with a 4-port transperitoneal access was used. 12-mm Hem-o-lok and titanium clips were used to secure the arteries. The left renal vein was typically secured with 2 Hem-o-lok clips, and in case of right laparoscopic donor nephrectomy the renal vein was typically secured with an Endo-TA multifire stapler. The extraction of the kidneys was performed via a flank incision of approximately 6 cm in length, then they were flushed with ice-cold histidine-tryptophan-ketoglutarate solution.
Renal Transplantation
Renal transplantation was performed by the standard extraperitoneal technique. Anastomoses between the renal vessels and the external iliac vessels were performed in an end-to-side technique. For ureteroneocystostomy, a ureteral JJ stent was routinely used. The stent was typically removed 6 weeks after transplantation.
Results
From 221 patients who underwent laparoscopic donor nephrectomy between 2011 and 2017, 11 (4.98%) showed the feature of a retroaortic left renal vein (Fig. 1). In 8 patients (72.7%) decision for left kidney donor nephrectomy was made.
CT scan of a retroaortic left renal vein. *, aorta; **, vena cava; →, retroaortic left renal vein.
CT scan of a retroaortic left renal vein. *, aorta; **, vena cava; →, retroaortic left renal vein.
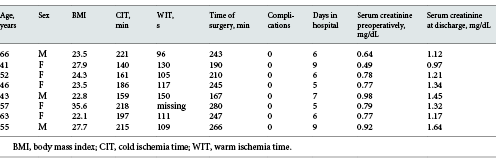
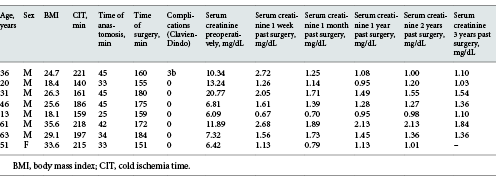
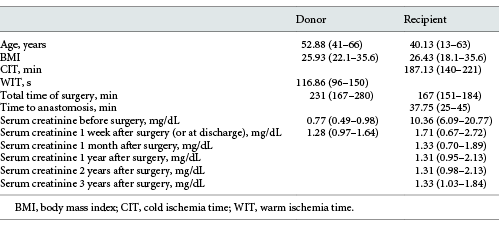
Detailed information about donors and recipients of these 8 cases are shown in Tables 1 and 2, regarding patient age, sex, body mass index (BMI), cold ischemia time (CIT), warm ischemia time (WIT), time of surgery, complications and serum creatinine at different times. The mean patient characteristics are shown in Table 3.
From donors who featured a retroaortic left vein, 3 (37.5%) were men and 5 (62.5%) women, with a mean age of 52.88 (41–66) years and a mean BMI of 25.93 (22.1–35.6). The mean time of surgery was 231 (167–280) min with an average WIT of 116.86 (96–150) s, whereas in 1 patient WIT was not documented. None of the patients showed postoperative complications higher than Clavien-Dindo grade 1 [6]. Their average hospital duration was 6.63 days (6–9 days). Overall mean preoperative serum was 0.77 mg/dL (0.49–0.98 mg/dL) and 1.28 mg/dL (0.97–1.64 mg/dL) at discharge.
Recipients were composed of 7 male (87.5%) and 1 female (12.5%) patients with a mean age of 40.13 years (13–63 years) and a mean BMI of 26.43 (18.1–35.6). Mean CIT was 187.13 min (140–221 min), mean surgery time for the recipients was 167 min (151–184 min) with an average time of anastomosis of 37.75 min (25–45 min). One recipient suffered a fascial dehiscence so that an operative revision was necessary.
Mean serum creatinine preoperatively, after 1 week, 1 month, 1, 2 and 3 years of follow-up was 10.36 (6.09–20.77) mg/dL, 1.71 (0.67–2.72), 1.33 (0.70–1.89), 1.31 (0.95–2.13), 1.31 (0.98–2.13) and 1.33 (1.03–1.84), respectively.
Discussion
The selection of potential donors for living kidney transplantation including the donor side is a complex responsibility. Every potential donor should get preoperative imaging to evaluate kidney anatomy and renal split function [7]. In case there is no relevant side-dependent difference in organ function or other advantages in retaining the left donor kidney, the left kidney is normally favored for transplantation due to the longer renal vein [8]. In the presence of anatomical anomalies, before choosing a side, a risk assessment for the donor and recipient has to be made.
Retroaortic left renal veins are reported to be present in 2–9% of living kidney donors [9-11]. Our hospital data match these results, with 11 patients (4.98%) who had a retroaortic left vein. Published research has listed the option to preferably choose a right donor kidney over a left in the presence of a retroaortic vein anomaly [12, 13]. Recent data from other authors suggest that choosing a left kidney with retroaortic vein is safe with good outcomes for donor and recipient [14-16].
This research shows the results of living donor transplantations of left kidneys with a retroaortic renal vein in Tables 1-3. From the study cohort, 8 identified patients showed this anatomical feature of whom none suffered any surgical complications. Furthermore, our current WIT, CIT, total time of surgery and transplant function results are all comparable to previously published results from our hospital [2, 17]. We did not perform any statistical analysis in this case study, since the cohort with 8 patients is very small compared to the overall 221 patients. In 3 cases with a present left-sided retroaortic vein, the right kidney was chosen solely based on the donor’s advantage retaining their left kidney.
The operative approach to the renal vein differs slightly in the presence of a retroaortic renal vein, since the vein enters the renal hilum inferiorly making the kidney less mobile. This often caries further anatomical variances including the entrance of lumbar, adrenal and gonadal veins. An advantage of this anatomical variance is the wider gap between the renal artery and vein due to their variable degrees of hilar entrance. The retroaortic renal vein is typically dissected from the lateral aortic border, thereby slightly shortening the total length which still exceeds the length of the right-sided renal vein.
Finally based on our data we conclude that living donor transplantation of a left kidney with a retroaortic vein anomaly can be performed without a higher risk for the donor and without potential disadvantages in transplant function for the recipient. The retrospective analysis as well as the limited number of patients might confound our results.
Conclusions
The identification and evaluation of a retroaortic left renal vein anomaly with a CT angiography and preoperative preparation is crucial for successful living donor transplantation. A retroaortic renal vein does not impact the perioperative outcome and hence displays no contraindication for donor and organ selection.
Acknowledgment
We cordially thank Antonia Wolf for carefully reading the paper.
Statement of Ethics
The data presented in this study were obtained ethically in accordance with the World Health Association Declaration of Helsinki. For retrospective analysis, patients were provided with a waiver with consent information. The study was approved by the ethics committee of Charité – Universitätsmedizin.
Disclosure Statement
All authors declare that they have no competing interests.
Funding Sources
There is no specific founding related to the subject matter of this article.
Author Contributions
Friedersdorff: designed the research study. Friedersdorff, Peters, Mang, Hennig: acquired the data. Mang, Friedersdorff: analyzed the data. Mang, Friedersdorff: wrote the paper. Biernath, Liefeldt, Bichmann, Ralla, Maxeiner, Peters, Cash, Budde: critically revised the paper.