Abstract
Introduction: This comprehensive review and meta-analysis investigates the effectiveness of neoadjuvant hormone therapy (NHT) in conjunction with radical prostatectomy (RP) for patients diagnosed with clinical stage T3 (cT3) prostate cancer (PCa) patients. Our objective is to evaluate its influence on cancer-related outcomes. Methods: In accordance with PRISMA standards, we conducted an analysis of 10 randomized controlled trials (RCTs) sourced from PubMed, Embase, Web of Science, and Cochrane databases, with a cutoff date of May 17, 2025. The main outcomes assessed included rates of positive surgical margins (PSMs) rates and prostate-specific antigen progression-free survival (PSA-PFS). Additional outcomes evaluated were pathologic complete response (pCR), minimal residual disease (MRD), and metastasis-free survival (MFS). We aggregated risk ratios (RRs), hazard ratios (HRs), and mean differences along with 95% confidence intervals (CI) utilizing either fixed or random-effects models. Results: The combination of NHT and RP led to a notable decrease in PSM rates when compared to RP alone (RR = 0.75, 95% CI: 0.60–0.94, p = 0.01), particularly evident in Asian demographics (RR = 0.47, p = 0.001) and for NHT durations of 6 months or more (RR = 0.75, p = 0.01). Additionally, PSA-PFS showed significant enhancement (HR = 0.25, 95% CI: 0.22–0.28). While there was no overall advantage in achieving pCR or MRD, certain subgroups in North America and those undergoing extended NHT experienced benefits. MFS did not show any significant changes (RR = 0.99, 95% CI: 0.89–1.10). Conclusion: The combination of NHT and RP enhances immediate surgical and biochemical results in patients with cT3 PCa, especially among those of Asian descent, and leads to a longer duration of NHT. However, the long-term survival advantages are still not established, highlighting the need for standardized RCTs to refine treatment protocols.
Introduction
Prostate cancer (PCa) represents a significant health issue and ranks among the most frequently diagnosed cancers in men globally. The disease exhibits a range of characteristics; some variants are slow growing and necessitate minimal treatment, while others are more aggressive, leading to considerable morbidity and mortality [1]. The financial impact of PCa goes beyond direct healthcare expenses, affecting patients’ overall well-being and placing a burden on healthcare resources. Available treatment modalities encompass radical prostatectomy (RP), radiation therapy, and various hormone therapies, each presenting unique benefits and drawbacks [2]. Despite progress in these therapeutic approaches, difficulties remain, particularly in addressing advanced cases such as clinical stage T3 (cT3) PCa, which continue to show elevated rates of positive surgical margins (PSMs) and biochemical recurrence [3].
Neoadjuvant hormone therapy (NHT) has been recognized as a promising strategy to enhance surgical results for individuals with locally advanced PCa [4]. The underlying goal of this treatment is to decrease tumor size and potentially lower the chances of PSMs during RP. Research findings on the impact of NHT on cancer outcomes have been inconsistent. While some studies indicate that it may improve disease-free survival rates, others report no notable advantages [5]. In particular, the effects of NHT warrant examination across various subgroups of PCa, with a focus on those identified as high risk.
The objective of this research is to assess how NHT affects surgical results in individuals diagnosed with cT3 PCa. Earlier studies have suggested that specific phenotypic traits, including tumor grade and prostate-specific antigen (PSA) levels, could affect the success of hormonal treatments [6]. Additionally, the link between the length of NHT and the status of surgical margins has been emphasized, indicating that extended treatment periods might lead to improved results [3]. This investigation aims to elucidate these connections and offer important perspectives on the role of neoadjuvant therapies in the management of PCa.
We will employ a structured methodology that includes a comprehensive review and meta-analysis of randomized controlled trials (RCTs) evaluating the efficacy of NHT alongside RP. This thorough approach facilitates the consolidation of data from various studies, thereby increasing the statistical strength and applicability of the results. Our goals are to evaluate the effects of NHT on PSM, PSA progression-free survival (PSA-PFS), pathologic complete response (pCR), minimal residual disease (MRD), and metastasis-free survival (MFS) within the specified patient group.
Methods
Protocol and Guidance
This systematic review and meta-analysis follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting systematic reviews and meta-analyses (online suppl. Table 1; for all online suppl. material, see https://doi.org/10.1159/000547875) [7]. Our protocol has been registered with the International Prospective Register of Systematic Reviews (PROSPERO, CRD420251042545).
Data Sources, Search Strategy, and Definitions
A thorough review of existing literature was conducted until May 17, 2025, utilizing the PubMed, Embase, Web of Science, and Cochrane databases. Our search incorporated terms such as NHT, RP, PCa, T3 PCa, advanced PCa, and oncological outcomes. To enhance our search, we also included synonyms related to these key concepts found in titles, abstracts, and keywords across the databases. Detailed search strategies for each database can be found in online supplement Table 2.
Study Selection: Inclusion and Exclusion Criteria
The studies included in this meta-analysis were chosen based on specific eligibility criteria established by the PICOS framework (Table 1). The criteria for inclusion were (1) Population (P): individuals diagnosed with cT3 PCa; (2) Intervention (I): NHT given before RP; (3) Comparator (C): individuals who had RP without prior NHT; (4) Outcomes (O): research that reported oncological results, such as PSMs, PSA-PFS, MFS, pCR, and MRD; (5) Study Design (S): only RCTs were considered. The exclusion criteria included (1) studies that did not explore the combination of NHT and RP in cT3 PCa patients; (2) non-randomized studies, such as observational studies, cohort studies, case reports, or review articles; (3) research that did not provide pertinent oncological outcome data or used inconsistent methods for measuring outcomes; (4) articles not published in English.
Study Selection and Data Extraction
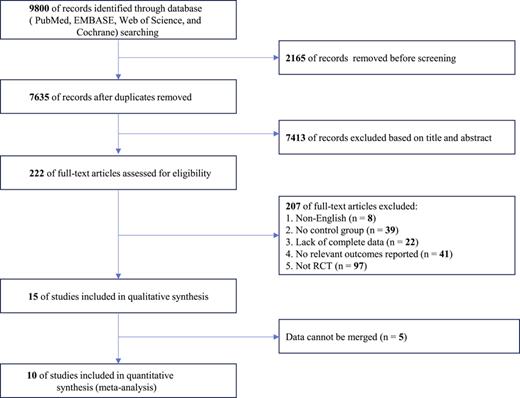
The flowchart illustrating the selection process of studies and the rationale for exclusions is depicted in Figure 1. Initially, duplicates were eliminated, followed by a review of titles and abstracts to assess their relevance. The full texts of the articles were then scrutinized for eligibility based on previously established criteria. Information gathered from each study encompassed the last name of the primary author, publication year, country of origin, research design, sample size, duration of treatment prior to surgery, age, diagnostic standards, and outcome metrics. Two authors (G.L., Y.L.) independently conducted the data extraction, and any differences were addressed through discussion or by consulting a third author (H.L.).
Risk of Bias Assessment
The Cochrane ROB 2 tool was utilized to evaluate the bias risk in the studies we included [8]. For each study, we made domain-specific assessments of bias risk, as detailed in the table below (Table 2). These assessments were derived from the information presented in each study, categorizing the bias risk as “low,” “high,” or “some concern.” Each study was assigned a classification of low risk, some concern, or high risk based on these evaluations, with explanations provided for each rating. A study is deemed low risk if randomization is executed correctly and there are no major issues with participant dropout or missing data. Conversely, if the randomization process lacks sufficient detail or if there are deviations in the intervention, we apply the ratings of some questions and clarify the rationale behind our judgment. A study is classified as high risk if randomization is inadequate or if there are significant biases due to selective outcome reporting or major flaws in the intervention. It is rated as high risk. Two authors (G.L., Y.L.) conducted independent evaluations of the study quality, and any disagreements were addressed with the assistance of a third author (H.L.).
Evidence Quality Assessment
This research utilized the GRADE (Grading of Recommendations Assessment, Development and Evaluation) framework to assess the quality of evidence concerning the primary outcome measures. The evaluation through GRADE was influenced by five factors that could lead to downgrading: bias in studies, inconsistency of results, indirectness, lack of precision, and publication bias. Each outcome’s evidence was categorized into one of four levels: “high,” “medium,” “low,” or “very low.” The assessment was conducted independently by two researchers, and the findings were compiled using GRADEpro GDT software (https://gradepro.org). If any disagreements arose, a third researcher was brought in to provide a resolution and facilitate consensus.
Statistical Analysis
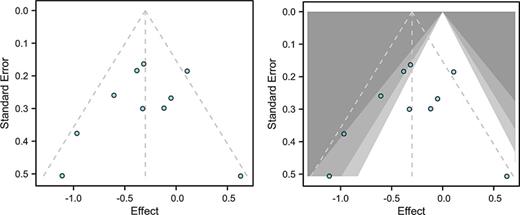
The analysis of data was performed utilizing Review Manager 5.3 software provided by the Cochrane Collaboration. The Q test was employed to evaluate heterogeneity among the studies, with a p value of less than 0.1 signifying notable heterogeneity. Additionally, the I2 statistic was applied, where an I2 value of 50% or higher indicated substantial heterogeneity. In cases of significant heterogeneity, a random-effects model was implemented; otherwise, a fixed-effects model was utilized. Subgroup analyses were carried out based on factors such as the country of origin, duration of treatment prior to RP, sample size, and the quality of the studies. A sensitivity analysis was performed using a leave-one-out method to determine the reliability of the results. To assess publication bias, Egger’s test, Begg’s test, and a visual examination of funnel plot asymmetry were conducted, with a p value of less than 0.05 deemed statistically significant.
Results
Study Selection and Characteristics
Initially, 9,800 studies were identified. We removed 2,165 duplicates and eliminated 7,413 articles through title and abstract screening. This process led to the retrieval of 222 full-text articles for further evaluation. After applying the specified inclusion and exclusion criteria, only 10 studies were selected for the final quantitative analysis. The exclusions were due to various reasons: 8 were non-English, 39 lacked a control group, 22 had incomplete data, 41 did not report relevant outcomes, 97 were non-RCT designs, and 5 had data that could not be combined (Fig. 1). Ultimately, the final selection consisted of ten RCTs, with two conducted in Europe [9, 11], two in Asia [12, 16], and six in North America [10, 13‒15, 17, 18]. The details of these 10 RCTs are summarized in Table 3.
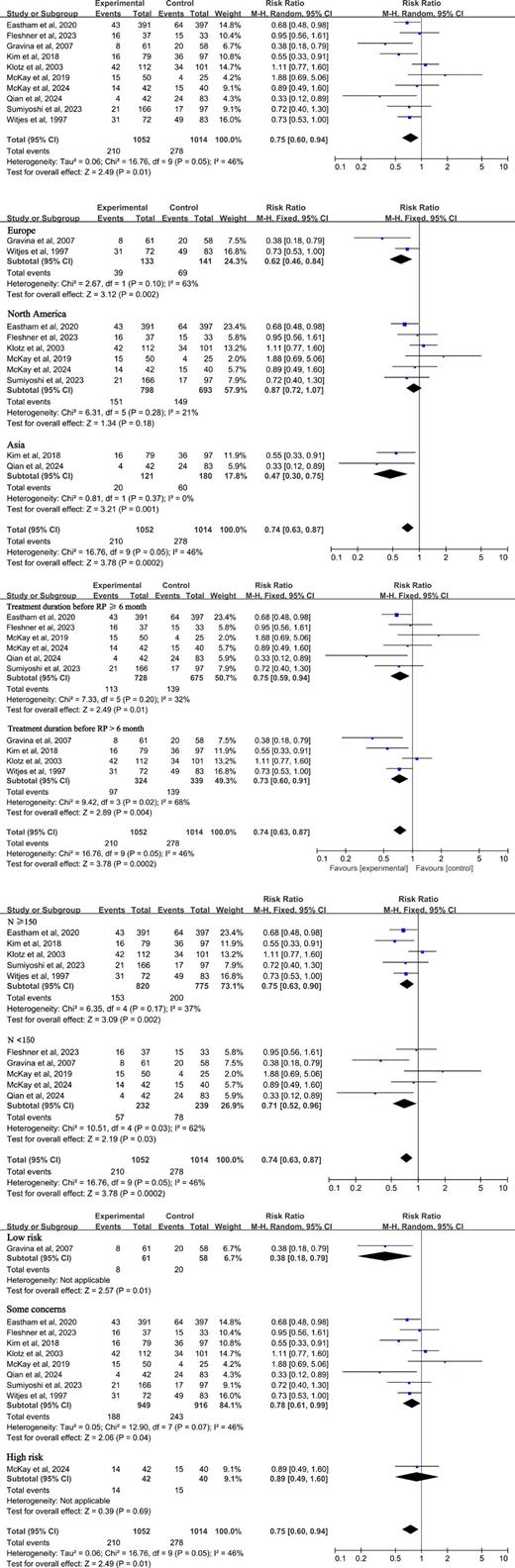
This meta-analysis encompassed ten studies that assessed the impact of NHT in conjunction with RP on PSM. The comprehensive evaluation revealed that the risk ratio (RR) for the combined treatment cohort was 0.75 (95% confidence intervals [CI]: 0.60–0.94, p = 0.01) (Fig. 2). A subgroup analysis was performed based on factors such as study design, duration of treatment, geographical location, sample size, and quality of the studies. Notably, studies conducted in Asia (RR = 0.47, 95% CI: 0.30–0.75, p = 0.001) and Europe (RR = 0.62, 95% CI: 0.46–0.84, p = 0.002) demonstrated significant advantages (Fig. 2). Both treatment durations of less than 6 months (RR = 0.73, 95% CI: 0.60–0.91, p = 0.004) and those of 6 months or more (RR = 0.75, 95% CI: 0.59–0.94, p = 0.01) exhibited noteworthy positive outcomes (Fig. 2). Studies with a sample size of 150 or more (RR = 0.75, 95% CI: 0.63–0.90, p = 0.002) and those with fewer than 150 participants (RR = 0.71, % CI: 0.52–0.96, p = 0.03) also indicated significant benefits (Fig. 2). Furthermore, studies with a low risk of bias (RR = 0.38, 95% CI: 0.18–0.97, p = 0.01) and those with some concerns (RR = 0.78, 95% CI: 0.61–0.99, p = 0.04) revealed significant effects (Fig. 2).
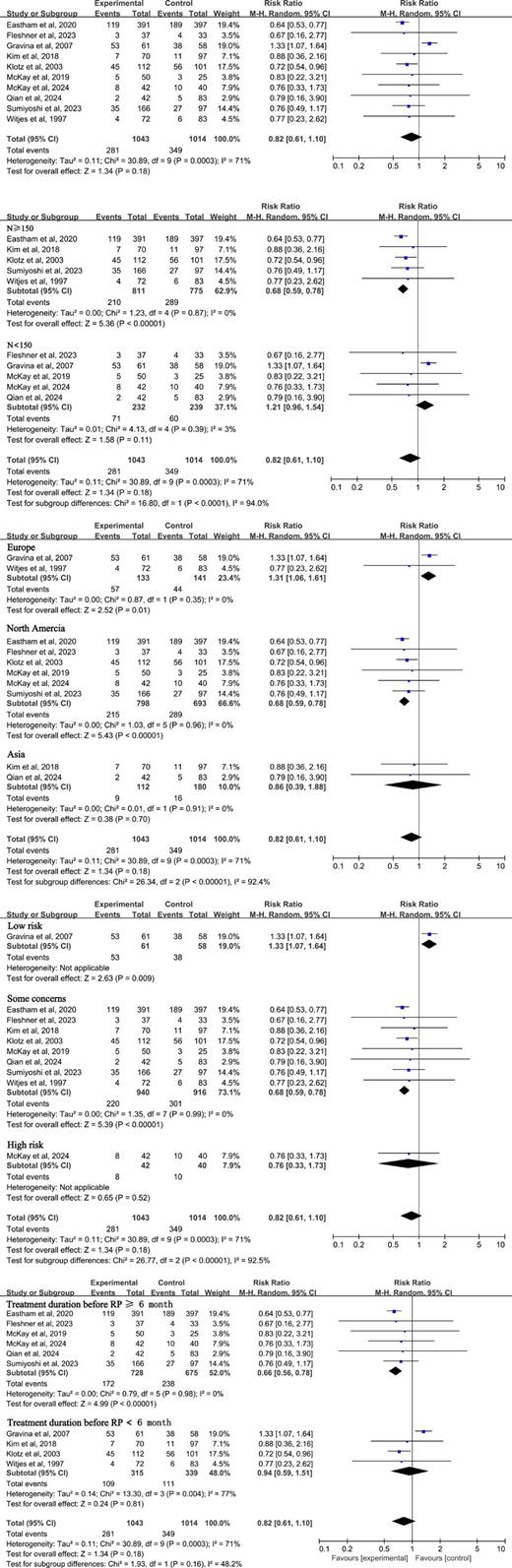
We conducted analysis of pCR following the combination of NHT and RP. The overall response rate was 0.82 (95% CI: 0.61–1.10), which suggests no notable difference in pCR (Fig. 3). In subgroup evaluations, studies with more than 150 participants indicated that the experimental group experienced significant advantages (RR = 0.68, 95% CI: 0.59–0.78, p < 0.01) (Fig. 3). The analysis by geographical region showed that the experimental group had considerable benefits in Europe (RR = 1.31, 95% CI: 1.06–1.61, p = 0.01) and North America (RR = 0.68, 95% CI: 0.59–0.78, p < 0.00001) (Fig. 3). In the risk stratification analysis, both the low-risk group (RR = 1.33, 95% CI: 1.07–1.64, p = 0.009) and certain concerns groups (RR = 0.68, 95% CI: 0.59–0.78, p < 0.00001) demonstrated benefits for the experimental group (Fig. 3). Additionally, patients undergoing treatment for more than 6 months exhibited significant advantages for the experimental group (RR = 0.66, 95% CI: 0.56–0.78, p < 0.00001) (Fig. 3).
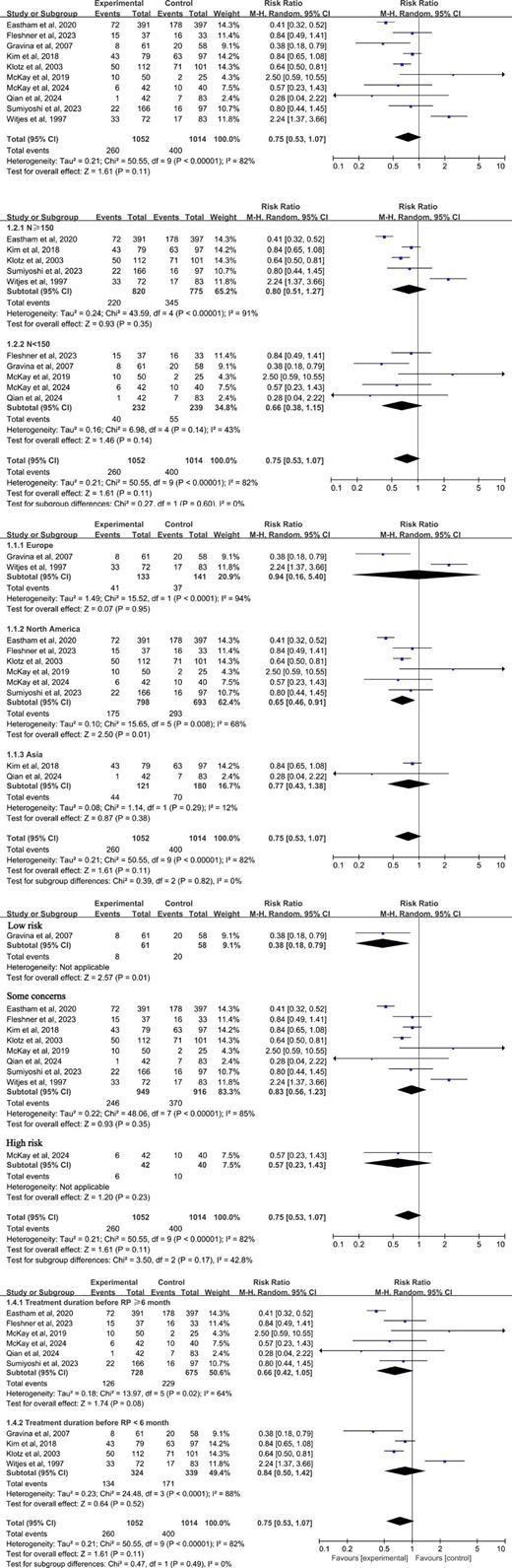
The overall RR for MRD was calculated at 0.75 (95% CI: 0.53–1.07), suggesting that there was no notable difference between the experimental and control cohorts (Fig. 4). This lack of significance persisted regardless of the sample size (Fig. 4). The analysis of MRD subgroups also revealed no significant differences based on sample size. However, in the North American region, the RR was 0.65 (95% CI: 0.46–0.91) (Fig. 4), while the low-risk subgroup showed an RR of 0.38 (95% CI: 0.18–0.79) (Fig. 4), and the subgroup with extended treatment duration had an RR of 0.41 (95% CI: 0.32–0.52) (Fig. 4). In these cases, the experimental group demonstrated significantly greater efficacy compared to the control group. Other subgroup analyses did not reveal any significant differences.
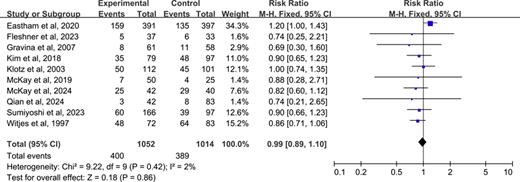
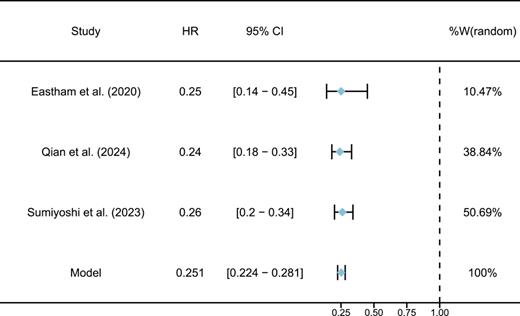
The overall RR for MFS was calculated at 0.99 (95% CI: 0.89–1.10), suggesting no notable difference between the groups receiving the experimental treatment and those in the control group (Fig. 5). We performed a meta-analysis to evaluate the impact of combining NHT with RP on PSA-PFS. The analysis included three qualifying RCTs (Eastham et al. [14]; Sumiyoshi et al. [17]; Qian et al. [16]) in the final quantitative assessment. As illustrated in Figure 6, the aggregated hazard ratio (HR) for PSA-PFS was found to be 0.25 (95% CI: 0.22–0.28), reflecting a significant decrease in the likelihood of PSA progression for patients who underwent NHT before RP. The tight CI and uniform effect sizes across reinforce the reliability of this result. Additionally, the heterogeneity was minimal, indicated by an I2 statistic of 0%.
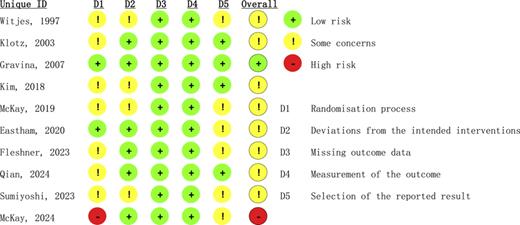
Risk of Bias
Out of the ten studies reviewed, just one was classified as having a low risk in every area assessed [11]. The majority, eight out of ten, were marked with “some concerns,” mainly concerning the methods of randomization and the reporting of outcomes. Additionally, one study was deemed high risk because of major problems with both randomization and the selection of outcomes (Fig. 7) [18].
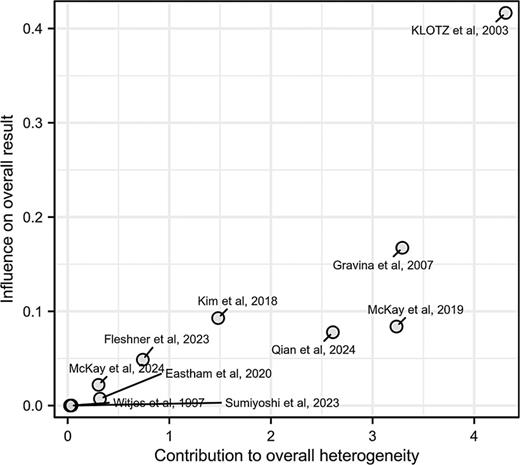
Sensitivity Analysis
To evaluate how bias risk affects the overall findings, we conducted sensitivity analyses. The results from the Baujat analysis (Fig. 8) and leave-one-out sensitivity assessments indicate that the meta-analysis results are strong and consistent across the majority of outcomes. The Baujat diagram highlighted Klotz et al. [19] as a significant factor contributing to both variability and overall effect size. Conversely, studies like McKay et al. [18] and Eastham et al. [14] had a negligible impact, suggesting a higher level of consistency. Additional sensitivity analyses reinforced there liability of outcomes such as PSM, MFS, and PSA-PFS, with no individual study significantly affecting the combined estimates. However, when Gravina et al. [11] and Witjes et al. [9] were excluded for pCR and MRD, respectively, there was a notable reduction in heterogeneity and the emergence of statistical significance, indicating these studies were major sources of variability. Overall, the findings affirm the dependability of the aggregated results.
Publication Bias Analysis
The findings from Egger’s regression and Begg’s rank correlation assessments revealed an absence of notable publication bias (Egger’s test: p = 0.5990; Begg’s test: p = 0.6547). Additionally, the trim-and-fill approach demonstrated that the overall effect size remained largely unchanged, reinforcing the reliability of our results (Fig. 9).
GRADE Evidence Quality Assessment
The primary outcomes were thoroughly assessed in this research utilizing the GRADE approach. Table 4 provides a comprehensive overview of the quality of evidence for each outcome measure. Notably, PSM is classified as high quality, PSA-PFS as medium quality, while the remaining outcomes are rated as low quality.
Discussion
PCa continues to be one of the most common cancers affecting men around the globe. It poses significant health challenges for patients and exerts considerable pressure on healthcare systems worldwide. The condition can advance to severe stages, such as metastatic cancer, which leads to elevated rates of illness and death. Although there have been improvements in treatment options, addressing high-risk, locally advanced PCa remains a complex issue. Existing treatment methods, including RP and various hormonal therapies, have limitations, especially regarding the recurrence of the disease and complications arising from treatment. This highlights the urgent need for new strategies to improve patient outcomes and alleviate these challenges [20, 21].
This research investigates the impact of NHT in conjunction with RP for patients diagnosed with cT3 PCa. We meticulously followed the PRISMA guidelines and employed comprehensive subgroup analyses to ensure the reliability of our results. Our primary outcomes indicate that NHT led to a 25% decrease in the PSM rate (RR = 0.75) and significantly enhanced PSA-PFS (HR = 0.25). The subgroup analysis highlighted that a duration of NHT of 6 months or more resulted in a more significant reduction in PSM rates. Additionally, there seems to be a trend indicating better treatment responses among Asian patients (RR = 0.47). While existing studies have shown varied outcomes regarding the advantages of NHT, often citing reductions in PSM and biochemical recurrence, many fail to consider the long-term survival impacts of this approach [22, 23]. Our meta-analysis fills a crucial void in the literature by integrating data from RCTs and illustrating that preoperative NHT markedly improves oncological results, particularly in lowering PSM rates. The findings align with the increasing agreement that NHT boosts the effectiveness of RP, particularly in high-risk, locally advanced cases of PCa [19]. Prior investigations, including those by Schow et al. [24] and Takamoto et al. [25], have examined different aspects of neoadjuvant therapies; however, our study offers a more comprehensive perspective by amalgamating findings from various trials to highlight the substantial advantages of NHT in enhancing surgical outcomes. In comparison to RP alone, NHT was linked to a decrease in PSM and an increase in PSA-PFS, reinforcing its significance in promoting long-term oncological management.
This research examines the cT3 subgroup, highlighting the ability of NHT to improve local control rates in patients with high-risk, locally advanced conditions. The RCTs included in the analysis showed that administering NHT for 6 months or longer led to a 25% decrease in the rate of PSM (RR = 0.75), suggesting that extended treatment periods may yield more pronounced effects on tumor control. This finding is consistent with the biological principles of androgen deprivation therapy, where blocking the androgen receptor pathway can trigger tumor cell apoptosis and diminish micrometastatic sites. The reduction in tumor size due to NHT likely lowers the chances of encountering PSMs during RP. Furthermore, the analysis of Asian subgroups revealed an impressive 53% enhancement in treatment effectiveness (RR = 0.47). This indicates that genetic and ethnic factors, such as variations in the androgen receptor pathway or differences in metabolism and endocrine responses, could affect how the Asian demographic responds to NHT, emphasizing the importance of considering these elements when customizing treatment plans for PCa.
Our research presents important insights for both clinical practice and health policy. It reveals that preoperative NHT provides considerable advantages for patients with cT3 PCa when compared to RP alone. The combined HR for PSA-PFS is 0.25 (95% CI: 0.22–0.28), suggesting that those who undergo NHT experience about a 75% lower risk of PSA progression than those who only have RP. While RP continues to be the primary treatment for clinically localized PCa, our results support the inclusion of NHT as a supplementary preoperative therapy. NHT improves biochemical control, potentially decreasing the chances of disease recurrence, which could lead to better long-term outcomes for patients. This aligns with the findings of Klotz et al. [19] and Fujimoto et al. [23], who recommend the adoption of new intervention strategies for high-risk patients to enhance long-term survival rates. Additionally, the studies analyzed show relatively tight CI and minimal heterogeneity, suggesting that these benefits are likely to be consistent across various populations. However, it is important to highlight that the study by Eshtem et al., which focuses on the North American demographic, contributes a lower weight to the pooled analysis (10.47%), possibly due to a smaller sample size or increased variability. This raises the possibility that the effectiveness of NHT could be affected by regional or demographic factors. From a health policy standpoint, the notable enhancement in PSA-PFS linked to NHT is significant. Given the consistent advantages demonstrated in three separate RCTs and the positive outcomes of the combined HR, there is a solid rationale for endorsing NHT as a standard part of preoperative care for cT3 PCa, particularly in healthcare systems focused on minimizing recurrence-related expenses and enhancing patients’ quality of life.
In addition to the notable effects on PSM and PSA-PFS, our research also investigated how NHT in conjunction with RP influences pCR. While the overall findings indicated that pCR did not achieve statistical significance (RR = 0.82, 95% CI: 0.61–1.10), certain subgroup analyses revealed beneficial effects of the combined treatment, particularly in studies with participant numbers exceeding 150 and those conducted in North America. In these specific groups, the enhancement in pCR may indicate the local control capabilities of NHT on tumors, especially among high-risk populations, implying that NHT could facilitate a favorable post-surgical pathological response by decreasing tumor size or modifying the tumor’s immune landscape. This observation aligns with the operational mechanism of NHT, which aims to diminish tumor size or alter the tumor microenvironment, thereby enhancing the chances of achieving complete remission. Furthermore, our analysis did not indicate a significant benefit of NHT combined with RP regarding MRD at this endpoint, with an overall RR of 0.75 (95% CI: 0.53–1.07), showing no notable difference between the treatment and control cohorts. Nevertheless, subgroup analyses of studies from North America, low-risk categories, and those with extended treatment durations revealed that the combined treatment group exhibited significantly improved outcomes. This suggests that MRD, as a clinical endpoint, may more accurately reflect treatment effectiveness in specific patient subsets, particularly those undergoing longer treatment regimens. Regarding MFS evaluation, the overall analysis did not demonstrate a significant impact of NHT combined with RP treatment on MFS (RR = 0.99, 95% CI: 0.89–1.10). This outcome indicates that, while NHT combined with RP may enhance local tumor control, reduce PSM, and improve PSA-PFS, its influence on metastasis control appears to be limited. This conclusion may align with existing research, which indicates that the effect of NHT on MFS remains ambiguous. Additionally, MFS could be affected by intricate factors such as tumor molecular features and the patient’s immune response.
The sensitivity analysis conducted in this research revealed significant variability in certain subgroup evaluations, particularly in metrics like PSA-PFS and pCR. Notably, the works of Gravina et al. [11] and Witjes et al. [9] played a major role in the overall variability observed in the pCR and MRD assessments. We believe this variability can be attributed to multiple factors. First, differences in NHT protocols among studies, such as the types of drugs used and the duration of treatment, may lead to varying effects. Second, the criteria for patient inclusion were inconsistent, especially across different regions and countries. Variations in initial patient characteristics, tumor stages, and PSA levels could greatly affect treatment outcomes. Lastly, discrepancies in the quality of studies and the sizes of the samples also contributed to this variability. To mitigate heterogeneity and yield more reliable findings in this area, future research should aim to standardize treatment protocols and patient inclusion criteria, alongside implementing larger international multicenter clinical trials.
It is important to recognize the constraints of our research. These constraints stem from the inconsistencies in treatment methods and results across the studies we reviewed. Variations in the duration of NHT and the criteria used for oncological evaluations complicate direct comparisons. Additionally, the limited number of participants in certain subgroup analyses, particularly within Asian populations, diminishes the strength of our conclusions and restricts our ability to make definitive statements. There is a clear need for longitudinal research to explore the long-term impacts and safety of combining NHT with RP, as pointed out by Miki et al. [26] and Stone et al. [27], who stress the importance of thorough assessments of neoadjuvant therapies.
In conclusion, this meta-analysis indicates that the combination of NHT and RP leads to significant enhancements in oncological results, particularly regarding PSM and PSA-PFS. However, the variability in outcomes and methodological challenges, including differences in study designs and participant numbers, call for careful interpretation of these findings. It is essential to take these elements into account when translating the results into clinical settings. Future studies should focus on conducting high-quality RCTs with uniform outcome metrics. This strategy will aid in refining criteria for patient selection and optimizing treatment plans, ultimately enhancing the management of advanced PCa.
Statement of Ethics
The Statement of Ethics does not apply in this case as the research relies solely on existing published works.
Conflict of Interest Statement
The authors declare to have no conflicts of interest.
Funding Sources
There was no funding for this study.
Author Contributions
Hua Luo was responsible for the conceptual framework, methodology, data management, writing, and oversight. Gaoyuan Liao and Yanghan Liu handled the methodology and were involved in the review and editing process. Gaoyuan Liao and Yanghan Liu made equal contributions to this project.
Data Availability Statement
The article contains all the data that were produced or examined throughout this research. For additional questions please contact the corresponding author.