Abstract
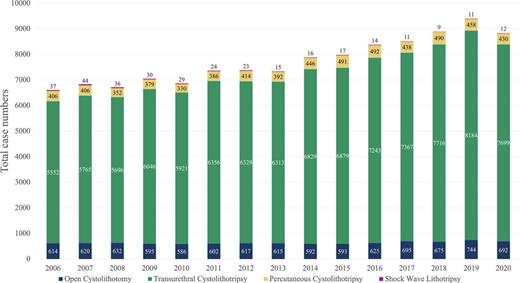
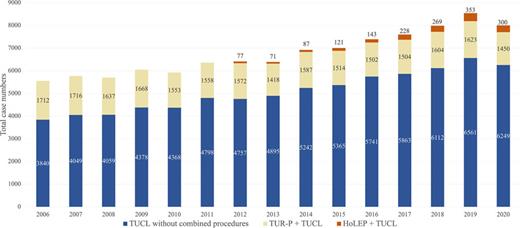
Introduction: The aim of the study was to analyze contemporary treatment trends in bladder stone management in Germany over a 15-year period. Methods: We analyzed data from the nationwide German hospital billing database from 2006 to 2020. The significance of changes over time was evaluated via linear regression analysis. Results: Total case numbers of therapeutic interventions for lower urinary tract calculi increased from 6,770 in 2006 to 9,037 in 2020 (p < 0.001). Transurethral cystolithotripsy (TUCL) was the predominant procedure with increasing case numbers from 5,552 in 2006 to 7,699 in 2020 (p < 0.001). Also, the share of TUCL increased by 4% during the study period. TUCL with laser fragmentation was coded in 82 cases in 2006 and in 1,527 cases in 2020 (p < 0.001). Case numbers of percutaneous cystolithotripsy also increased over time from 406 to 430 cases (p = 0.005), but the share decreased by 20%. Inpatient shock wave lithotripsy is very rarely performed for bladder calculi with an average of 22 cases per year in all hospitals in Germany. Case numbers of open cystolithotomy (OCL) also increased from 614 cases in 2006 to 692 cases in 2020 (p = 0.006), but the share decreased by 15.5%. On average, 164 cases of stone removal from neobladders per year were performed, mainly transurethrally (47%) or via an open approach (21%). Case numbers of TUCL combined with transurethral resection of the prostate (TUR-P) declined from 1,712 in 2006 to 1,450 in 2020 (p = 0.014). However, this might be attributed to the concomitant rise of laser enucleation of the prostate with steadily increasing case numbers in Germany. Conclusion: We present contemporary population-based data on bladder stone treatment in Germany. TUCL is the predominant therapeutic modality with increasing case numbers, but OCL is still performed frequently. TUR-P is the procedure that is most often combined with TUCL.
Introduction
The discovery of a bladder stone in an ancient Egyptian mummy dating back 5,000 years ago is a testimony to the long struggle of humankind with lower urinary tract calculi [1]. Hippocrates was the first to describe symptoms of bladder stones, but surgical treatment was frowned upon and eventually forbidden to perform for physicians, as outcomes were dismal in ancient times [2]. With the advent of endourology, things changed dramatically [2]. Bladder stones account for approximately 5% of all urinary stones in humans [3]. The etiology of bladder calculi is multifactorial, and in industrialized countries, they typically occur in elderly patients due to foreign bodies, obstruction, urinary stasis, or infection with a male predominance [4].
Medical treatment of bladder calculi is an option for patients with suspected or confirmed uric acid stones and is comprised of alkalization of urine following the treatment regimen of uric acid stones in the upper urinary tract. However, this is infrequently performed as it is time consuming, backed with little evidence and arguably associated with low success rates [5, 6].
Minimally invasive treatments such as transurethral cystolithotripsy (TUCL), percutaneous cystolithotripsy (PCCL), shock wave lithotripsy (SWL) as well as laparoscopic/robot-assisted cystolithotomy have emerged and represent valuable alternatives to open suprapubic cystolithotomy (OCL). Donaldson et al. [7] demonstrated in a systematic review and meta-analysis that both TUCL and PCCL are associated with shorter hospital stays, faster convalescence, and shorter catheterization time with comparable stone-free rates (SFRs) when compared to OCL. Mechanical, laser, pneumatic, ultrasonic, and electrohydraulic lithotripsy is available for fragmentation. However, reliable evidence on the best method is lacking. Stone formation in patients after continent urinary diversion is a dreaded long-term complication after cystectomy and often requires transurethral or open surgical removal of the stone. The aims of this study were to assess current treatment patterns for lower urinary tract calculi in adults and to present population-based data from Germany on lower urinary tract calculi over a 15-year period.
Materials and Methods
German Hospital Billing Database (Diagnosis-Related Groups)
A total population analysis of the nationwide billing data in Germany from 2006 to 2020 was performed. The reimbursement of inpatient treatment in Germany is regulated by the diagnosis-related groups. A specific ICD-10 (International Statistical Classification of Diseases and Related Health Problems) diagnosis code and an OPS (German adaption of the International Classification of Procedures in Medicine) code for the performed intervention compose the specific diagnosis-related group. Data locally stored at the select hospital are transferred to the Institute of Hospital Remuneration and finally to the German Federal Statistical Office (Destatis). Patients treated exclusively in psychiatric and forensic facilities as well as military personnel treated in military hospitals are not included in this analysis. All other patients that underwent inpatient treatment in Germany are represented in the nationwide Destatis database. Thus, this database can be regarded as complete for the given purpose. Our group has described the methodology used for this work in detail [8].
Specific ICD-10 codes for lower urinary tract calculi were combined with OPS codes for diagnostic and therapeutic procedures to assess bladder stone-specific surgeries. Detailed information on the methodology is provided in online supplementary Tables S1, S2 (for all online suppl. material, see https://doi.org/10.1159/000542750).
Data Protection and Ethics Statement
We followed the “REporting of studies Conducted using Observational Routinely collected health Data” (RECORD) statement and performed all actions in accordance with the Declaration of Helsinki in its latest version [9]. Analyzed data were completely anonymized and derived from established databases with rigorous data protection measures. Therefore, an additional ethics statement was not required.
Statistics
We extracted the absolute number of cases as well as the length of hospital stay (LOS) with SAS V9.4 (SAS Institute, Cary, NC). The results were stratified for patient characteristics and surgical approach. To compare rates and means, we implemented the χ2 test or Wald tests. Linear regression analysis for trends over time was performed with SPSS 29.0.1.0 (IBM Corp., Armonk, NY). We defined p < 0.05 to indicate statistical significance.
Results
Unless otherwise noted, all trends refer to the total study period from 2006 to 2020. Total case numbers of therapeutic interventions for lower urinary tract calculi increased from 6,770 in 2006 to 9,037 in 2020 (p < 0.001). The mean shares of the procedures during the study period were as follows: TUCL 84.3%, PCCL 5.3%, OCL 8%, SWL 0.3%, and removal of bladder calculi from a continent urinary diversion 2.1%.
TUCL was the most frequent procedure to remove bladder calculi in the observed time frame in Germany. Case numbers of TUCL significantly increased from 5,552 to 7,699 (p < 0.001). Also, the share of TUCL increased by 4% during the study period. In total, 87% of patients were male and the mean age was 69.3 ± 13.7 years at time of TUCL. The mean length of stay for TUCL was 6.3 ± 10.2 days (7.8 days in 2006 vs. 5.4 days in 2020). The use of laser fragmentation for bladder calculi increased from 1.5% in 2006 to 19.8% in 2020. The shares of TUCL performed with laser fragmentation during the study period increased from 1% (2006) to 25% (2020, p < 0.001).
Case numbers of PCCL slightly increased over time from 406 cases to 430 cases (p = 0.005), but the share decreased by 20%. Overall, 89% of patients were male and the mean age was 69.2 ± 14.4 years at time of PCCL. The mean length of stay for PCCL during the study period was 8 ± 8.9 days (9.5 days in 2006 vs. 5.7 days in 2020). In 2008, only 12 PCCL cases (3.4%) were coded with laser, whereas 85 cases (19.8%) were performed with laser in 2020 (p < 0.001).
Case numbers of inpatient SWL for bladder calculi were low and significantly declined from 37 cases to 12 cases per year (p < 0.001). Totally, 87% of patients were male and the mean age was 65.9 ± 17 years at time of SWL. The mean length of stay for SWL during the study period was 7.1 ± 7.6 days (9.1 days in 2006 vs. 4.6 days in 2020). On average, 22 cases of inpatient SWL for lower urinary tract stones were performed in all hospitals in Germany per year.
Case numbers of open cystolithotomy (OCL) significantly increased from 614 to 692 cases (p = 0.006), but the share decreased by 15.4%. A total of 88% of patients undergoing OCL were male, and the mean age was 68.9 ± 15.6 years at time of OCL. The mean length of stay for OCL during the study period was 13.1 ± 11.1 days (14.9 days in 2006 vs. 11.6 days in 2020). Robotic cystolithotomy was very rarely performed with 4 cases in 2015 and 24 cases in 2020.
Total case numbers of TUCL, PCCL, OCL, and SWL are shown in Figure 1. Case numbers of stone lithotripsies in neobladders significantly increased from 120 to 151 cases (p = 0.004) resulting in an overall stable share for bladder stone treatments of 2.1% on average. Calculi in the neobladder were most commonly removed transurethrally (43/120 cases in 2006, i.e., 36% vs. 71/151 cases in 2020, i.e., 47%). An open approach was used in 39/120 cases in 2006 (32.5%) and 34/151 cases in 2020 (22.5%). PCCL in the neobladder was rarely performed with 10 cases in 2006 and 12 cases in 2020.
During the study period, 25% of TUCL was performed in combination with either TUR-P, holmium laser enucleation of the prostate (HoLEP), thulium laser enucleation of the prostate (ThuLEP) or transurethral resection of a bladder tumor (TUR-B) (Fig. 2). Case numbers of TUCL combined with transurethral resection of the prostate (TUR-P) declined from 1,712 in 2006 to 1,450 in 2020 (p = 0.014). Generally, cases numbers for TUR-P performed for benign prostate hyperplasia (BPH) declined from 57,914 cases in 2006 to 41,583 cases in 2020. Hence, in 3.5% of all TUR-P cases a TUCL was performed and 18.8% of all TUCL cases were combined with TUR-P in 2020.
Conversely, we observed a concomitant rise of HoLEP with steadily increasing case numbers from 2,263 cases in 2012 to 7,811 in 2020 (p < 0.001). Also, the numbers of TUCL combined with HoLEP increased from 77 cases in 2012 to 300 cases in 2020 (p < 0.001). In 4% of all HoLEP cases, a TUCL was performed and 3.9% of all TUCL cases were combined with HoLEP. Also, a steady increase in ThuLEP case numbers was observed with 2,146 cases in 2018 (which was the first year with a specific ICD code available) and 2,778 in 2020. Sixty-nine ThuLEPs were combined with TUCL in 2018 (3.2%) and 91 in 2020 (3.3%). Case numbers of internal urethrotomies declined from 41,391 cases in 2006 to 22,728 in 2020 (p < 0.001). Likewise, also case numbers of internal urethrotomies combined with TUCL declined from 779 cases in 2006 to 612 in 2020 (p < 0.001). A total of 102,738 TUR-B cases were recorded in 2006 and 116,932 in 2020. Overall, 247/102,738 (0.2%) TUR-B were combined with TUCL in 2006 and 306/116,932 (0.3%) in 2020. Case numbers of simple prostatectomy (SP) for BPH declined from 6,300 cases in 2006 to 3,228 cases in 2020 (p < 0.001). In 2006, 183 cases of SP were combined with OCL (2.9%) and 190 cases in 2020 (5.9%). Vice versa, in 27.5% of all OCL cases it was combined with SP. Case numbers of patients with neurogenic bladder dysfunction and bladder stones who underwent TUCL increased from 279 cases to 330 cases (p < 0.001).
Discussion
We present contemporary population-based data on the management of lower urinary tract stones in Germany over a period of 15 years. Total case numbers of surgical interventions for bladder calculi significantly increased over time, which is mainly attributed to the increase in TUCL. TUCL case numbers significantly increased from 5,552 in 2006 to 7,699 in 2020, and the share of TUCL of all interventions increased by 4%. We saw a shorter LOS for TUCL (6.3 days) compared to PCCL (8 days). This finding is in accordance with a recently published meta-analysis of 4 RCTs, also showing a shorter LOS for TUCL (mean difference was 0.82 days) and faster convalescence when compared to PCCL [7]. However, transurethral manipulation may still be an issue as stricture rates after transurethral stone fragmentation and removal range from 2.9% to 19.6% [7, 10]. Thus, percutaneous suprapubic cystolithotripsy is especially favorable in patients where urethral trauma needs to be avoided (e.g., artificial urinary sphincters or after buccal mucosa grafts). Convalescence and hospital stay tend to be shorter with TUCL [7]. For major postoperative complications and retreatment rates, no significant differences were found [7, 11, 12].
SWL represents the least invasive operative approach to bladder stones not necessarily requiring general anesthesia. Reported SFR for SWL for bladder calculi ranges from 78 to 94% [13‒15]. However, most studies are dated and retrospective in design. When compared to TUCL, Ali et al. [15] showed that multiple SWL sessions are needed in order to reach similar SFRs. The uncommonly prolonged LOS for SWL could be caused by a combination of multiple sessions of inpatient SWL into 1 patient case as sometimes performed in clinical practice. Another explanation might be the selection of cases with complications (e.g., hematoma/hemorrhage/sepsis/obstruction) which could entail prolonged stays. However due to anonymization regulations, these theories cannot be verified. In Germany, SWL for bladder calculi was very rarely performed in an inpatient setting with only 22 cases on average per year in Germany. The declining application of SWL for upper tract stones and easy access to endourologic therapies might trigger underutilization [16]. Reimbursement in Germany does not differ for SWL, TUCL, and PCCL; hence, cost should not be a factor in choosing the treatment modality [17]. On the other hand, in a previous study from our study group we were able to demonstrate that the share of SWL for upper tract stones as an outpatient procedure increased in contrast to the declining numbers of inpatient SWL [16]. This might also be a reasonable scenario for bladder stones. However, due to lack of outpatient data we cannot test this theory for the present study.
Of the surgical approaches, OCL had the longest LOS when compared to TUCL, PCCL, and SWL, which is not surprising as it is the most invasive procedure. Nevertheless, in patients with very high stone burden and/or patients where transurethral and percutaneous access is not advisable or feasible, OCL is still a valuable approach to extract bladder calculi.
In accordance with upper tract calculi treatment, laser technology has also found its way in the treatment of bladder stones. In 2006, the use of laser fragmentation was only coded in 82 cases of TUCL (1.5%), whereas in 2020 almost 20% were performed using laser energy. This development is in accordance with the implementation of new lasers such as the holmium:yttrium-aluminum-garnet laser and the thulium fiber laser [18].
In 18.8%, TUCL was combined with TUR-P and in 3.9% with HoLEP. The acquired data for this study are comparable to the data retrieved for a previous work regarding the operative therapies for BPH in Germany [19]. OCL was combined with SP in 27.5% of cases. However, we could not assess how many patients underwent TUCL and desobstruction in separate stays. In Germany, hospitals can bill 2 separate cases after a minimum waiting period of 30 days. We hypothesize that hospitals may tend to split these cases into two separate interventions and hospital stays.
The incidence of stone formation in continent urinary diversions (orthotopic neobladders, heterotopic pouches) in current literature is around 5%, being slightly higher than in our collective [20, 21]. Different patient populations investigated likely cause this difference. In some patients, these stones cause hematuria, dysuria, lower abdominal pain, or recurrent urinary tract infections [22]. However, in order to preserve continence, according to Patel et al. [23], aggressive instrumentation of the urethra or ileal nipple in case of a catheterizable pouch should be avoided. In cases with larger calculi, an open approach might be advisable to achieve complete stone clearance. In Germany, approximately 7,200 cystectomies are performed each year and in about 29% of these patients a continent urinary diversion (27% orthotopic neobladder, 2% catheterizable continent pouch) is created [24, 25]. The incidence of calculi in a continent urinary diversion of 2% would translate into about 97 cases of stones per year. However, we observed a mean number of 164 cases per year during the study period. About half of those are managed transurethrally and 23% via an open approach.
To our knowledge, this is the first report of population-based data on bladder calculi in Germany and the European Union giving insights in current usage of the various treatment modalities. Since bladder stone treatments are oftentimes regarded as interventions with low skill requirement or even a by-product of further endoscopic interventions, not much attention is paid to the incidence or the development of these procedures. Our results show that bladder stones are a relevant aspect of everyday clinical practice and therefore also a cost factor in Western healthcare systems. The continuously increasing number of cases over the past 2 decades also demonstrates a perspective of increasing importance for the future. The underlying cause for the surge of interventional bladder stone therapies remains unclear, but demographical changes with an aging population might be the main contributor. We could demonstrate a slight increase in patients with neurogenic bladder dysfunction and bladder calculi who underwent TUCL.
The main study limitations can be derived from the nature of the data itself. Although billing data convey a high degree of accuracy, clinical information on number and size of bladder calculi is not available. Thus, information on additional factors such as indwelling catheters, stone composition, and size or other patient-derived factors could not be assessed. In addition, we cannot provide data on all of the lithotripsy modalities used, as only usage of lasers can be coded separately. Also, we cannot provide data on outpatient procedures which might affect mainly SWL case numbers. Due to German data protection regulations, single patients or institutions may not be identified and all outcomes are limited to the inpatient stay. Nevertheless, the presented data are comprised of all patients who underwent inpatient treatment for bladder calculi in German hospitals and can be regarded as complete for the given purpose.
Conclusion
We present contemporary population data on bladder stone interventions in Germany. TUCL is the predominant therapeutic modality accounting for about 84% of all bladder stone interventions with increasing case numbers in the observed time period. PCCL is a minimally invasive alternative with a share of 5% of all bladder stone surgeries. With a share of 8%, OCL has become a less frequently used approach. Inpatient SWL is very rarely performed for bladder calculi in Germany. When TUCL is combined with desobstruction of the prostate, TUR-P is the most common transurethral procedure.
Acknowledgments
German research data center of the federal statistical office, DRG-statistics 2006–2022, own calculations. We thank Janina Loske for supporting data retrieval. This project was developed within the framework of the working group “Health Services Research, Quality and Economics” of the DGU e.V.
Statement of Ethics
Written informed consent to participate in the study was not required in accordance with local/national guidelines. Ethical approval is not required for this study in accordance with local and national guidelines. All statistical procedures were in accordance with the ethical standards of the institutional and/or national research committee and with the declaration and its later amendments or comparable ethical standards.
Conflict of Interest Statement
Dr. Johannes Huber reports grants and nonfinancial support from Intuitive Surgical, Takeda, Janssen, APOGEPHA, Bayer, and Coloplast outside the submitted work. Dr. Groeben reports fees by Janssen, MSD, and Merck Pharmaceuticals outside the submitted work. All other authors have no conflicts of interest to declare.
Funding Sources
This study was not supported by any sponsor or funder.
Author Contributions
Roman Herout: project development, data analysis, and manuscript writing. Angelika Borkowetz, Juliane Putz, and Martin Baunacke: data analysis and manuscript editing. Rainer Koch: data extraction and analysis. Christian Thomas: supervision and manuscript editing. Johannes Huber: project development, supervision, and manuscript editing. Christer Groeben: project development, data analysis, supervision, and manuscript editing.
Data Availability Statement
The data that support the findings of this study are not publicly available due to the anonymization regulations of the German Federal Office of Statistics (Destatis). Output records and calculated tables are available from the corresponding author [R.H.].