Abstract
Amputation of the testis is very rare in clinical situations; therefore, most surgeons have no experience with an amputated testis. In this case, a 31-year-old male with schizophrenia amputated both testes due to self-mutilation. We performed replantation surgery via microscopy. On postoperative day 1, he removed his right testis by using his hand, even though his hands were restrained. The second attack disrupted the viability of the right testis. However, after proper management, we checked the normal sex hormone level by preserving the replanted left testis. We evaluated the viability of the replanted testis by performing five examinations, namely, intraoperative indocyanine green injection, testicular scan with technetium pertechnetate, contrast-enhanced computerized tomography, Doppler ultrasonography, and serum testosterone level. In this report, we aimed to describe our rare experience about management with replantation of the amputated testes and evaluation of their viability.
Introduction
Amputation of the testis is rare in clinical situations. Thus far, less than 30 cases have been reported in the literature [1, 2]. In our institute, 1 patient with completely amputated testes and scrotal skin through self-mutilation was admitted in 2022. He self-amputated his testes twice in 2 consecutive days. In this report, we aimed to describe our rare experience about management with replantation of the amputated testes and evaluation of their viability in a patient with schizophrenia who has severe psychotic symptoms but refused proper psychiatric treatment.
Case Presentation
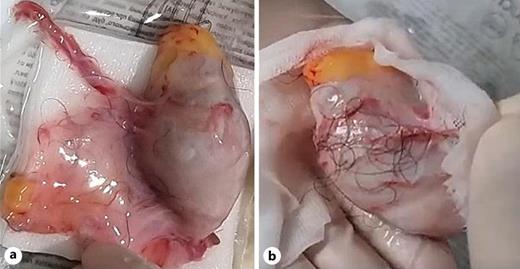
A 31-year-old unmarried male patient was diagnosed with schizophrenia. He was treated with clozapine for 10 years, but his psychiatric symptoms were poorly managed because he arbitrarily reduced dose of clozapine. He and his family were offered hospitalization and treatment, but they refused. In the past 2 months, he has experienced auditory hallucination and delusion of being controlled by a microchip in his body. He amputated his testis and scrotal skin with scissors. According to the patient, he had both testicles amputated because he thought a chip inside the body directed it. His family brought him to our hospital with the amputated tissues in normal saline in a plastic bag with ice (Fig. 1). During physical examination in our emergency room, he had stable vital signs, but he had bleeding with arterial pumping in both spermatic cords; for this reason, compression by gauze packing was performed. During preparation for surgery for about 2 h, computerized tomography (CT) was checked to exclude other injuries. Hemoglobin decreased from 14.1 g/dL to 12.2 g/dL.
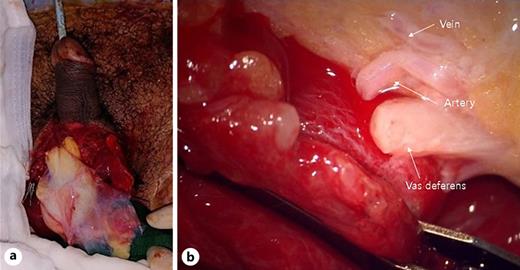
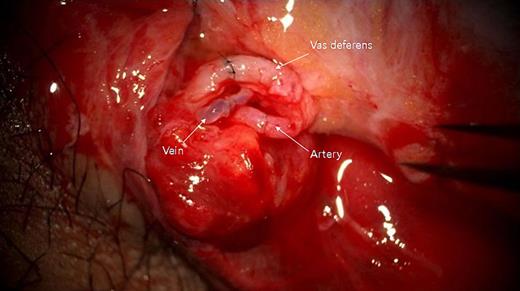
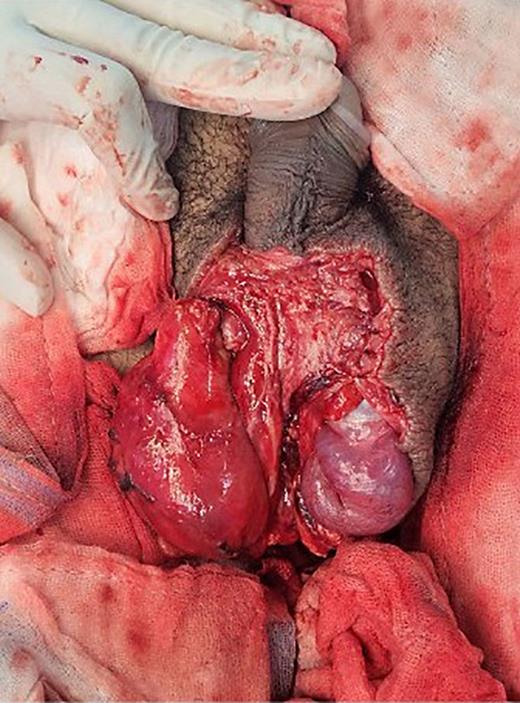
Cooperative surgery was performed by surgeons from the urology and plastic surgery departments. The patient was placed supine in a frog-leg position. The proximal gonadal artery in the spermatic cord was detected easily with pulsating bleeding and secured by clamping without causing vessel injury (Fig. 2). The vas deferens was also found near the gonadal artery with a resilient tactile sense. Thin lumens around the gonadal artery were identified as gonadal veins. The amputated testis was also checked, and the vas deferens was continued from the tail of the epididymis. The gonadal artery was located in the same direction as the vas deferens. The testis was fixed on the scrotal wall to prevent it from roaming freely. The gonadal artery was first connected using 11-0 nylon under an operating microscope (KINEVO 900, Zeiss; Fig. 3). After vein drainage was confirmed, gonadal vein anastomosis was performed with 11-0 nylon (Fig. 3). Lastly, two-layer vasovasostomy was carried out with 8-0 nylon (Fig. 3). After the end-to-end anastomosis of the artery, vein, and vas deferens, the viability of the testis could be confirmed in terms of vascularity on gross and indocyanine green fluorescence perfusion (Fig. 4). The cremasteric muscle of the spermatic cord was reinforced to reduce tension in the anastomosis sites, and orchiopexy was performed to prevent testicular torsion. The other testis was replanted in the same maneuver (right testis: artery 1ea, vein 1ea; left testis: artery 1ea, vein 2ea). The ischemic time of each testis was 7 h (right) and 8.5 h (left). Each testis was raised on a high scrotal area and fixed with the approximated dartos fascia because of the large skin defect of the scrotum (Fig. 5). Lastly, the amputated scrotal wall after defatting was used to cover the whole defect.
After the surgery, both of his hands were restrained in the bed because he was considered to have high risk of reattempt of self-harm based on his recent attempt at severe self-injury and persistence of auditory hallucination and delusion of being controlled. However, on postoperative day (POD) 1, he self-amputated his right testis by using his hand. During the preparation for re-operation, his hemoglobin decreased to 6.4 g/dL, and blood pressure was unstable despite normal saline and transfusion (2 pints). Because of self-amputation, ischemic time could not be checked precisely. In the operating room, the amputated tunica albuginea turned to a dark color. Even though warm saline was irrigated, an advanced ischemic change could not be reversed (Fig. 6a). The artery was clamped, and the grafted skin was resized to allow perfusion of more blood supply (Fig. 6b). Additional packed red blood cells and fresh frozen plasma (4 pints each) were transfused. Thus, his hemoglobin reached 12.5 g/dL.
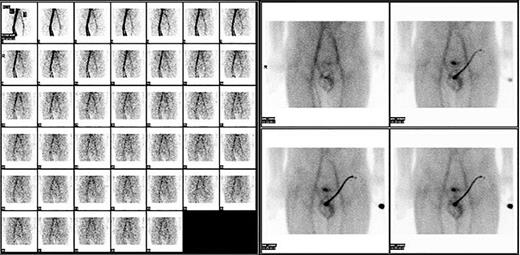
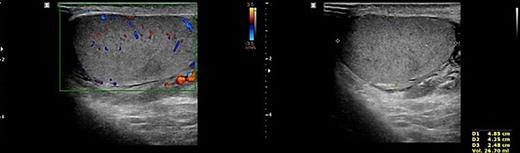
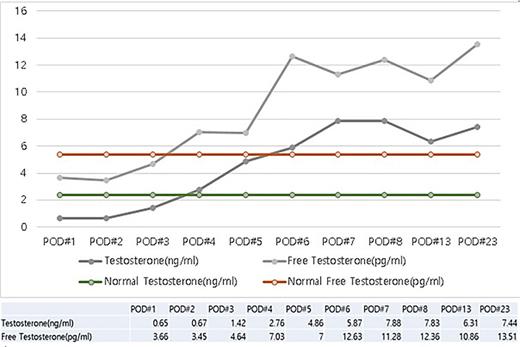
To prevent the patient from further self-injury, simple therapeutic restraint of both arms was performed with the patient’s consent, and sedative medication was administered. He was closely observed in the intensive care unit to monitor his hemoglobin and systemic conditions. Additional transfusion treatment was provided as needed. Psychiatric medicines including antipsychotics and sedatives (Clozapine 125–250 mg/day, haloperidol 2.5–5 mg, and lorazepam 1–2 mg/day) were prescribed by a psychiatrist. After 5 days of taking the psychiatric medication, the patient no longer reported the impulse to harm himself, and was able to release the simple restraint on both arms. No further self-harm occurred until he was discharged, presumably due to the proper effects of taking psychiatric medication. Anticoagulant agents (5 mg apixaban, twice per day), subcutaneous heparin injection (5,000 IU, twice per day), and alprostadil (10 mg, once per day) were given for circulation to prevent the thrombosis of vessels. On POD2 from the first operation, a testicular scan with technetium pertechnetate revealed the viability of the remnant left testis compared with the amputated right testis (Fig. 7). On POD4, contrast-enhanced CT showed the enhancement of the vessel into the testis (Fig. 8). On POD7, scrotum Doppler ultrasonography revealed the Doppler signal in the parenchyma of the testis (Fig. 9). Testosterone levels increased after the surgeries and normalized on POD5 (Fig. 10). He was discharged on POD9 without any skin complication (Fig. 6c). After discharge, he returned to our clinic for follow-up on POD13 and 23. On the visit, laboratory follow-up including testosterone and free testosterone was checked and confirmed as normal (Fig. 10).
Discussion
The testis has two main functions, namely, making sex hormones and producing sperm. Loss of both testes is related to loss of sexual and reproductive functions, which can decrease the quality of life and cause psychological difficulties in men, especially sexually active young men. For alternative approach instead of replantation surgery, simple testosterone supplementation and ligation of the vas could be the option. However, testosterone supplementation may be an option for checking testosterone level after replantation. Also, testosterone supplementation may cause adverse effect due to controlling hormones in the hypothalamus and pituitary [3]. Loss of bilateral testis means loss of spermatogenesis and fertility. It may be an ethical or legal problem to give up and only administer male hormone supplementation therapy, even though it can save the testicles in patients with accidently damaged testicles. Even if there was another risk of self-amputation, young and healthy patients who had a chance to control his psychiatric problem could be the indication for this surgery. Also, his family strongly desired prompt treatment of replantation surgery. We thought that replantation should be the first choice in consideration of patients’ physical and psychological aspects, family support, and medical ethics. However, few cases of amputation of the testis have been reported; therefore, most surgeons have no experience with amputated testes [1, 2]. In previous two care reports, the mechanism of injury involved self-amputation and trauma such as wrong-site surgery [1, 2].
In this report, an extremely rare case of a serial amputation attempt of the testis because of a psychological condition was presented. The patient was diagnosed with schizophrenia and had uncontrolled severe psychotic symptoms. He did self-injury by burning himself with a cigarette in a few weeks before admission and by cutting off his testis just before admission, indicating that he was at a high risk of re-attempting self-harm [4, 5]. Recent self-harm in patients with schizophrenia is known as a risk factor for reattempts of self-harm, in addition to the high levels of past or recent suicidal thoughts; past episodes of depression, substance abuse, or dependence; and increased number of psychiatric hospitalizations [4]. In this case, the patient self-injured the next day after surgery and removed the testis on the right side. Therefore, if possible, surgeons should consider replanting both testes. If similar cases are documented, a protocol for the restoration of both testes of a psychologically impaired patient can be considered.
Self-amputation is characterized by a clearly cut plane without any hesitation. In this case, the amputated testis had a simple and clear-cut plane. The right testis had long remnant vessels and vas deferens, which could help detect the anatomical parts and anastomose easily. Although the left testis had extremely short vessels and vas, these parts could be connected via microscopy, and the testis was recovered. Testicular vascular supplies are composed of the gonadal (testicular) artery from the aorta, the vasal artery from the internal iliac artery, and the cremasteric artery from the inferior epigastric artery [6]. Among them, the gonadal artery was the main supply source [7]. One gonadal artery was anastomosed, and the testis survived with normal testosterone levels.
After serial events of self-amputation, one testis was saved. Testicular torsion managed by orchiectomy or orchiopexy can result in reduced sperm concentration, motility, or normal morphology, which is indicated by anti-sperm antibody production or reperfusion damage on the contralateral testis [8]. In a previous study, testosterone levels were lower in the orchiectomy group than in the salvaged group after testicular torsion, but the seminal and erectile functions were not significantly different between the groups in 1–4 years of follow-up [9]. The paternity of men with a single testis is not diminished compared with that of the general population [10]. In cases with loss of testicular function, testosterone replacement therapy is needed for hypogonadism [1].
We performed five examinations to check the viability of the replanted testis. First, in the operating room, we used indocyanine green after replantation (Fig. 4). Indocyanine green fluorescence perfusion showed testicular perfusion, which enabled the immediate checking of the viability of vessels. This procedure is appropriate for checking the viability of microscopic vessels that may be damaged during a milking test. Second, a testicular scan showed the viability of the testis (Fig. 7). One testis is markedly different from the lesion of orchiectomy. However, the scan resolution was low because of a wide range of arterial courses and the disturbance of the urethral catheter or bladder. Third, contrast-enhanced CT displayed the vascularity of the testis and the surrounding parts (Fig. 8). However, the shooting time to the enhanced phase could affect the failure of the vascularity of the testis. No protocol for this case has been established in our institute; therefore, CT was a nonspecific tool for testicular examination. Fourth, ultrasonography efficiently showed the vascularity inside the testis (Fig. 9). However, skin wound could inhibit or limit ultrasonography. Fifth, we indirectly checked the testicular function based on testosterone levels (Fig. 10). A laboratory examination should be performed continuously. However, this procedure could be limited among hypogonadal men, and the separate testicular function of each testis could not be easily identified. Nevertheless, these techniques will help determine the viability of the testis in specific situations.
On microscopic surgery, to prevent anastomotic blood vessel blockage, anticoagulation therapy was used. We used NOACs (non-vitamin K antagonist oral anticoagulants, apixaban) for their safety. It is known that it has advantages over standard agents, such as warfarin, for fewer drug interactions, rapid onset, and short half-lives. Comparing the study with warfarin in atrial fibrillation, it showed lower side effects on stroke events and major bleeding [11]. Heparin is widely used in micro-anastomosis surgery for its effect on preventing both arterial and venous thrombosis acting. Adequate dose of heparin is known to be safe and effective in vessel-anastomosis surgery [12]. Prostaglandin E1 (PGE1, alprostadil) is used for treatment of vessel claudication and peripheral arterial occlusive disease. It has vasodilation, antithrombotic, anti-ischemic, and anti-inflammatory effects. In microscopic surgery including anastomosis, PGE1 is used in prevention and treatment of spasm and thrombosis [12].
Various postoperative management methods should be performed. First, the patient is likely to induce self-harm at any time; therefore, sedative treatment with physical restraints should be actively considered. After the first operation, the patient suffered serial self-injury when only physical restrictions were provided; however, after the second operation, the testis was successfully preserved when the patient was stabilized by sedation [13]. Second, as amputation cases are accompanied by massive bleeding, hemoglobin levels and the overall condition of the patient must be closely monitored, and active blood transfusion treatment is required. Third, if the anastomotic blood vessel is blocked, the testicles must be removed; thus, an anticoagulant should be used, and testicular evaluation should be performed [12]. Lastly, in the case of amputation due to self-harm, surgeons from several departments must treat patients in a multidisciplinary way rather than taking responsibility for all of them in one department. In this case, since psychosis was the main cause of the problem, it was essential to manage psychiatric symptoms through consultation with the department of psychiatry.
Statement of Ethics
All procedures performed in this study were in accordance with the ethical standards of the Institutional and/or National Research Committee(s) and with the Helsinki Declaration (as revised in 2013). This study was approved by the Chung-Ang University Hospital Institutional Review Board (IRB approval number: 2210-012-19441) and was conducted in accordance with Declaration of Helsinki provisions.
Written informed consent for publication of this case report and accompanying images was obtained from the patient. A copy of the written consent is available for review by the editorial office of this journal.
Conflict of Interest Statement
The authors declare no conflicts of interest.
Funding Sources
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (NRF-2022R1A2C2008207).
Author Contributions
Conception, design, and data analysis and interpretation: Se Young Choi and Shin Hyuk Kang. Administrative support and provision of study materials or patients: Il Young Ahn and Moon Soo Ha. Collection and assembly of data: Woo Ju Kim and Sun Mi Kim. Manuscript writing and final approval of manuscript: Il Young Ahn, Moon Soo Ha, Woo Ju Kim, Tae Hui Bae, Sun Mi Kim, Se Young Choi, and Shin Hyuk Kang.
Data Availability Statement
The data used to support the findings of this case report are included within the article. Further inquiries can be directed to the corresponding author.
References
Additional information
Il Young Ahn and Moon Soo Ha contributed equally to this work as the co-first authors.