Abstract
Background: Complex soft tissue defects involving the lower abdomen, perineum, and groin (LAPG) represent reconstructive challenges following urologic surgery. Consequently, these often require an interdisciplinary approach involving plastic surgery. While pedicled flaps from the lower abdomen are a reliable option, previous placement of colostomies and urinary urostomies renders these flap types unavailable. Here, the pedicled anterolateral thigh perforator (ALT) flap represents a reliable pedicled alternative which can harvest from the thigh. Materials and Methods: A retrospective data analysis of pedicled perforator flaps harvested from the thigh to reconstruct soft tissue defects was conducted. Seven patients treated in the urology department with soft tissue defects following tumor resection, infection, and dehiscence were included. Results: In all patients, the ALT flap was utilized successfully to reconstruct soft tissue defects up to 450 cm2 in size. All flaps survived. In 1 case, prolonged wound healing was observed. All defects were adequately addressed with no recurrence of dehiscence or fistula formation. Conclusions: Pedicled perforator flaps represent a valid option for the soft tissue reconstruction of the lower abdomen and perineum when a pedicled rectus abdominis flap is no longer available. This flap is, therefore, a good option in an interdisciplinary approach to soft tissue reconstruction, especially following urologic surgery, which is predominantly performed in the LAPG region.
Background
Complex, large soft tissue defects resulting from infection, radiation, or tumor resection of the lower abdomen, perineum, and groin (LAPG) region represent a rare challenge in reconstructive urology [1, 2]. These full-thickness defects mandate expeditious treatment to reconstruct the functional integrity of the LAPG unit, retain organs, and cover neurovascular structures [3, 4]. Soft tissue reconstruction may require an interdisciplinary approach involving surgical specialties such as plastic surgery [5]. While microvascular tissue transfer has evolved tremendously over the past few decades and has revolutionized soft tissue reconstruction in many areas, the LAPG region remains a domain of pedicled flaps, because reliable alternatives (such as muscle-based flaps) exist [6-8]. The vertical rectus abdominis myocutaneous flap is a versatile and reliable flap. However, it may not be available in patients with previous abdominal surgery including colostomies and urostomies, as its perfusion through the deep inferior epigastric artery is based on the integrity of the muscle [9, 10]. Also, the harvest of a muscle results in a loss of function at the donor site. In case of the rectus abdominis muscle, laxity of the abdominal wall and even hernia formation have been reported [3]. With the advent of perforator-based pedicled flaps, the anterolateral thigh flap (ALT), which is harvested from the upper thigh in close proximity to the LAPG region, has been added to the armamentarium of the reconstructive plastic surgeon [9]. A perforator-based flap is a fasciocutaneous flap based on a vascular pedicle which is elevated by a retrograde intramuscular dissection. Any perforator can serve as a vascular pedicle if adequate length can be obtained and the donor site is aesthetically and functionally acceptable [11]. Here, the ALT flap is most commonly supplied by the musculocutaneous (ca. 85–90%) or septocutaneous (ca. 10–15%) perforators of the descending branch of the lateral circumflex femoral artery (LCFA), which can be dissected with ease by an experienced surgeon due to consistent anatomy. However, scarce anatomical variations (e.g., transversal branches of the LCFA) can exist and should, therefore, be considered during planning and the surgical procedure itself [7].
While raising a pedicled perforator flap such as the ALT flap is technically significantly more challenging than harvesting a muscle flap, patients benefit from a reduced donor site morbidity as muscle is spared, which results in reduced functional deficits [11]. Additionally – unlike the vertical rectus abdominis myocutaneous flap – the pedicled ALT flap is available in patients with previous abdominal surgeries [3, 4, 7]. Since tissue defects in reconstructive urology often involve the LAPG region, we reviewed our experience with the pedicled ALT flap for the reconstruction of these often complex soft tissue defects in the present study.
Materials and Methods
Study Design
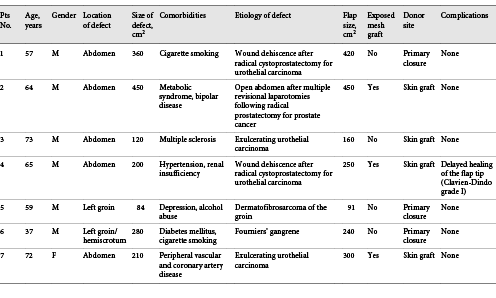
A retrospective study was conducted to evaluate the reliability, versatility, and reach of the pedicled ALT flap in an interdisciplinary setting. Patients undergoing soft tissue reconstruction with a pedicled ALT flap from April 2014 to April 2020 were identified by chart review. Only patients initially treated by the department of urology which were subsequently referred to the plastic surgery service for extensive soft tissue reconstruction were included. Data extracted from the patient charts included age, gender, comorbidities, the etiology, location and size of the defect, presence of infection, presence of synthetic mesh material, size, and location of the flap, closure of the donor site, and postoperative complications.
Operative Approach
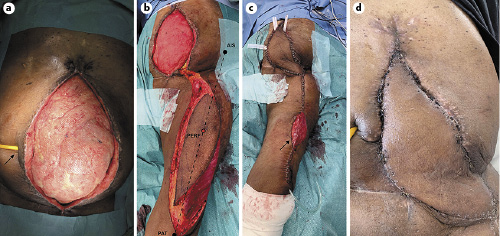
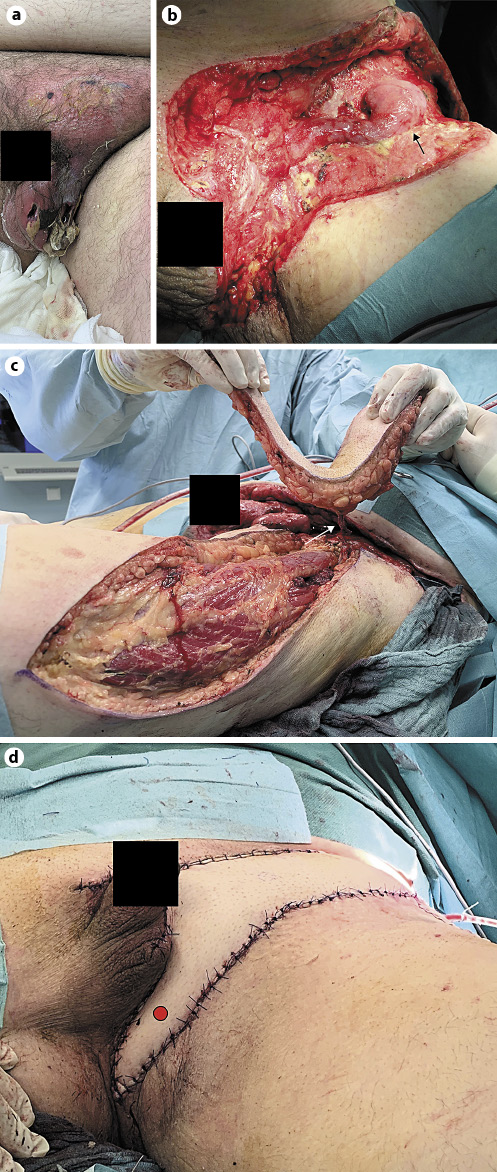
Flap transfer was planned as soon as the soft tissue defect was debrided thoroughly or adequate margins for tumor resection were achieved (Fig. 1a, 2a, b). Patients with prior soft tissue surgeries at the anterior thigh and vascular surgery in the pelvis did not qualify for a perforator flap. The locations of the perforating vessels at the donor site were preoperatively mapped with a handheld Doppler probe. A thought line connecting the anterior superior iliac spine and the lateral superior pole of the patella was marked (Fig. 1b). Around its midpoint within a circle of 3 cm diameter, perforators are most commonly encountered. The outline of the flap exceeding the size of the defect by 1 cm to all sides was then eccentrically placed over the dominant perforator. Intraoperatively, an exploratory incision is placed along the medial side of the flap to gain access to the subfascial plane, where the perforator was visualized (Fig. 2c). Once deemed adequate to serve as the vascular pedicle, reevaluation of the flap outline was performed to confirm that the perforator entered the flap at its cranial border. When centering the flap outline over the perforator, reach of the pedicle is reduced. The perforator was then microsurgically dissected under loupe magnification in a retrograde fashion through the vastus lateralis muscle up to its origin at the descending branch of the LCFA. All side branches were clipped or ligated to allow tension-free mobilization of the pedicle. Once adequate pedicle length was confirmed, the flap was transferred into the defect (Fig. 1c, 2d). Especially in periumbilical abdominal defects, additional length of the pedicle can be gained by tunneling the flap underneath the rectus femoris and sartorius muscle. After inset of the flap, the donor site was closed primarily if flap width did not exceed 8 cm; larger flaps required a skin graft at the donor site (Fig. 1c). Postoperatively tension and compression of the vascular pedicle and flap were minimized by 5 days of bed rest. During this time, an antibiotic prophylaxis is carried out with a 5-day intravenous treatment of a third-generation cephalosporin.
Results
The clinical demographics of the patients are presented in Table 1. Seven patients were included in the present analysis. Six patients were male, 1 female with an average age of 61 years. The etiology of the defects was preceding surgery for muscle-invasive urothelial carcinoma in 4 cases and surgery for prostate carcinoma or dermatofibrosarcoma of the left groin in 1 case each. In 1 other case, the defect resulted from surgery for Fournier’s gangrene. Surgical mesh grafts following preceding surgery were exposed in 3 cases. The size of the defect averaged 243 cm2 ranging from 84 to 450 cm2. The size of the flap ranged from 91 to 450 cm2 (average 273 cm2). The donor site could be closed primarily in 3 cases, 4 patients required a skin graft. All flaps survived; in 1 case, prolonged healing of the tip of the flap occurred. No fistula formation was encountered postoperatively (Fig. 1d). All patients ambulated after 5 days of bed rest. No complications at the donor site were noted.
Discussion
Tumor resection, wound dehiscence infection, and trauma of the LAPG region may result in extensive, full-thickness soft tissue defects [5, 12, 13]. This can often be the cause of unexpected early mortality [14]. To retain abdominal or pelvic organs, the reconstruction of a mechanically stable abdominal wall or pelvic floor is mandatory [9, 12]. While a reconstruction with a surgical mesh and secondary skin grafting of granulation tissue may work, common complications are chronic infections eventually requiring complete removal of mesh grafts [13]. Here, vascularized soft tissue reconstruction with pedicled flaps bears advantages with regard to the aesthetic result as well as the mechanical integrity of the abdominal wall and pelvis [5, 6]. As only few pedicled flaps exist which can be used in this region, large defects sometimes require free tissue transfer [6]. Despite microvascular tissue transfer being a safe and reliable option, it adds operative time and requires meticulous postoperative monitoring in the immediate postoperative phase [7, 15]. The pedicled ALT flap allows transfer of a large flap with the inclusion of the fascia lata, which not only adequately addresses the soft tissue defect but also allows closure of the fascial defect with autologous fascia and may obviate the need for surgical mesh [7, 9, 16-18]. The results of this study add comprehensive evidence regarding safety and reliability of the pedicled ALT for large and complex LAPG defects in an interdisciplinary setting. All patients had multiple surgeries prior to soft tissue reconstruction. In such complicated cases, autologous tissue transfer is required to address these extensive defects. The rectus abdominis flap is often a reliable and good option for perineal defects unless placement of a colostomy or urostomy through the anterior abdominal wall may have jeopardized its perfusion [3, 5]. Concerning this, the pedicled ALT flap can be used if the rectus flap is unavailable [9, 15, 17]. In addition, another advantage of the ALT flap is the preservation of functional integrity of the abdominal wall [3]. The upper thigh as a donor site is also well accepted by most patients despite its visibility [7, 10]. Flap harvest spares the posterior thigh, gluteal region, or back, which should be avoided as a donor site in these often nonambulatory or bedridden patients to prevent formation of pressure sores at the donor site. The ALT flap can be harvested up to a size of 35 × 25 cm based on a single perforating vessel [11, 15, 17]. No other locally available flaps can supply vascularized tissue of this extent. Only free flaps such as the latissimus dorsi muscle flap or the scapular flap may be harvested in similar dimensions [6]. The pedicled ALT flap represents a perforator flap which requires meticulous perforator dissection without the need for a microvascular anastomosis [10, 11]. In experienced hands, flap harvest is rapid and may be incorporated in a simultaneous primary tumor resection and soft tissue reconstruction procedures [4, 9]. This is advantageous for the patient as it reduces the number of surgeries. As a limitation, the reach of the pedicled flap might be inadequate for supraumbilical defects [17, 18]. Here, a number of technical modifications have been introduced to extend the reach of the flap such as tunneling the vascular pedicle under the rectus femoris muscle and the sartorius muscle [18]. This has been routinely and safely performed in this study to reach both high abdominal and perineal defects. Other options are the eccentric flap planning with regard to the perforating vessel as well as slightly bending the hip in the initial postoperative period to take tension off the pedicled flap [18]. While the first is often applied, the latter is not well tolerated by elderly patients and may complicate postoperative mobilization. A major advantage of using pedicled flaps in an interdisciplinary setting is that postoperative monitoring of perfusion is simple and does not require highly trained staff such as in free tissue transfer [5].
Conclusions
As a general rule for soft tissue defects in operative urology, a plastic surgeon should be involved if the defect cannot be readily covered with simple skin advancement flaps or other commonly used techniques. Here and especially for the LAPG region, we show that the pedicled ALT flap allows expeditious soft tissue reconstruction of large and complex soft tissue defects after urologic surgery while sparing the muscular integrity of the abdominal wall. It, thus, can be safely utilized in an interdisciplinary setting.
Statement of Ethics
All the findings, data acquisition, and processing in this study comply with the ethical standards laid down in the latest declaration of Helsinki of the World Medical Association as well as with the statutes of the Ethics Committee of the University of Würzburg concerning anonymized retrospective medical studies. Thus, a separate ethics vote was not necessary. All involved patients gave their written and informed consent for the publication of their anonymized cases.
Conflict of Interest Statement
None declared.
Funding Sources
No external funding was used for the creation of this manuscript.
Author Contributions
R.J., M.J., and C.K. conceived of the study, performed surgery, and wrote the manuscript. A.V., A.K., and H.K. were involved in the data acquisition, surgical procedures, and manuscript editing. C.K. created all figures.